

Diagnosis: Peritonsillar abscess
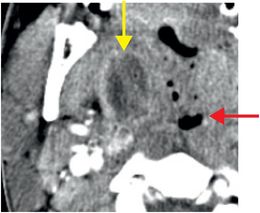
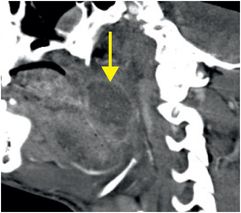
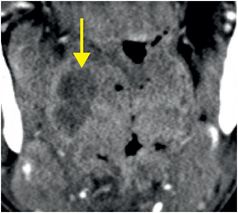
Axial (left), sagittal (middle), and coronal (right) contrast-enhanced CT images show a large, peripherally enhancing abscess in the region of the lateral right pharynx (yellow arrows) at the level of the tongue. The abscess is in the region of the right palatine tonsil at the level of the oropharynx (red arrow).
Discussion
Peritonsillar abscess is usually caused by tonsillitis and resultant suppuration, which occurs most commonly in young adults.
Historically known as quinsy, a peritonsillar abscess may be suspected in a patient with fever, odynophagia, cervical adenopathy, and a “hot potato” (muffled) voice.
While children have a high prevalence of pharyngotonsillitis, abscess formation is more commonly seen in young adults. Risk factors for abscess include upper respiratory infection, alcohol, smoking, recent dental procedure, and immunosuppression.
Trismus, due to spasm of the adjacent medial pterygoid muscle, is generally not seen in tonsillitis, but is common in peritonsillar abscess. This distinction is key because tonsillitis is usually diagnosed clinically and treated with antibiotics only, while peritonsillar abscess is often diagnosed on imaging and is treated with incision and drainage in addition to antibiotics.
Anatomy of cervical fascial planes and routes of spread of infection are important to evaluate for potential complications.
The peritonsillar space is partially encircled posteriorly and laterally by the superior pharyngeal constrictor muscle. If infection penetrates this muscle and its surrounding pharyngobasilar fascia, bacteria may spread to adjacent cervical spaces.
The retropharyngeal space (posteromedial), carotid space (posterior), parapharyngeal space (posterolateral), and masticator space (lateral) are suprahyoid neck spaces encircled by layers of the deep cervical fascia. Any of these spaces may become secondarily involved (schematic of deep neck spaces is provided below).
Self-assessment
|
|
|
|
|
|
Relevant anatomy
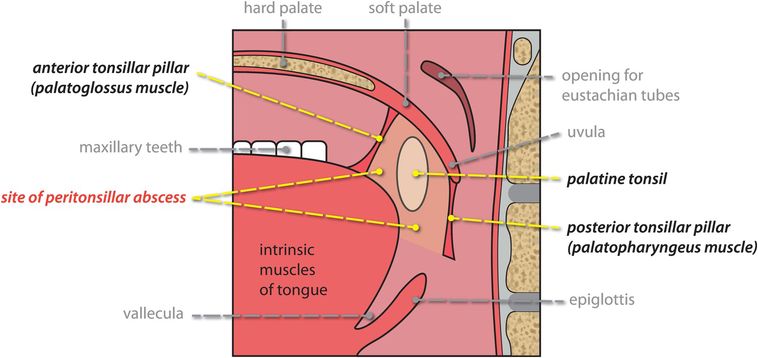
Sagittal schematic demonstrates the anatomy of the peritonsillar space.
The peritonsillar space is defined by loose connective tissue that surrounds the palatine tonsil, and is bounded front-to-back by the anterior tonsillar pillar (the palatoglossus muscle, connecting the soft palate to the tongue) and the posterior tonsillar pillar (the palatopharyngeus muscle, connecting the soft palate to the pharynx).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








