
Diagnosis: Intracranial abscess due to sinusitis
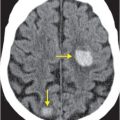
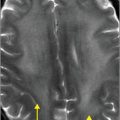
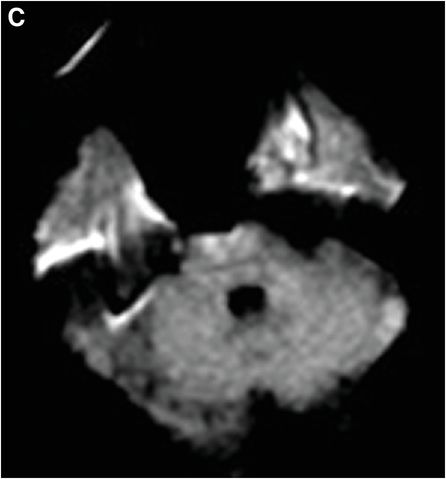
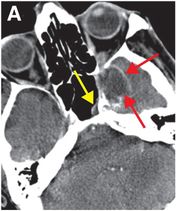
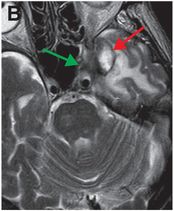
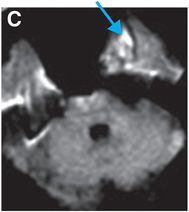
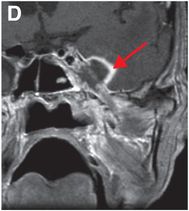
Axial contrast-enhanced CT (A) shows partial opacification in the left sphenoid sinus (yellow arrow) and a ring-enhancing abscess (red arrows) in the left middle cranial fossa. On axial T2-weighted (B), axial diffusion-weighted imaging (DWI; C), and coronal contrast-enhanced T1-weighted MR (D), the rim of the abscess demonstrates T2 shortening and enhancement (red arrows). Internal contents show abnormal signal on DWI (blue arrow). Low signal in the left cavernous sinus on T2-weighted imaging is suggestive of fungal invasion (green arrow).
Discussion
Overview of sinusitis
Sinusitis or rhinosinusitis is a common disease that affects 30–37 million patients annually in the US. It is the fifth most common reason for antibiotic prescription.
Sinusitis is caused by the inflammation of the lining of the sinuses due to blockage of mucous drainage. Patients are predisposed by upper respiratory infection, allergies, polyps, and deviation of the nasal septum. Risk factors for sinusitis include immunocompromise, autoimmune disease, cystic fibrosis, and exposure to second-hand cigarette smoke. The majority of cases of acute sinusitis (70–80%) are caused by viral infection. Bacterial infection (30% of cases) is caused by organisms such as Haemophilus influenzae, Streptococcus pneumoniae and Moraxella catarrhalis.
Symptoms of sinusitis include facial pain/pressure, congestion, nasal discharge, headache, cough, toothache, anosmia, and halitosis. Bending over or lying down may exacerbate symptoms. Maxillary sinusitis is often due to odontogenic etiology.
Acute sinusitis is defined as infection lasting up to 4 weeks.
Subacute infection lasts 4–12 weeks, and chronic, greater than 12 weeks.
Patients with recurrent sinusitis have 4 or more separate episodes of acute sinusitis within one year.
Sinusitis due to viral respiratory infection is usually self-limited, lasting 7–10 days, while bacterial infections last for more than 10 days.
Fungal sinusitis
Fungal sinusitis is a more serious illness often encountered in immunocompromised patients with conditions such as AIDS, stem cell or organ transplant, and diabetes.
Allergic non-invasive fungal sinus disease is more prevalent in patients with asthma and nasal polyposis.
Complications of sinusitis
Untreated or aggressive sinusitis can progress to involve the frontal bone (otherwise known as Pott’s puffy tumor – a condition characterized by osteomyelitis and subperiosteal abscess in children) or orbits.
Intracranial involvement of aggressive sinusitis includes meningitis, epi- or subdural empyema, intracranial abscess, and occasionally cavernous sinus thrombosis either by direct infectious extension or via emissary and diploic veins.
About 10% of intracranial abscesses are due to sinus infection, occurring most commonly in young men. Infectious organisms travel either by direct extension or via the valveless venous system that connects sinus mucosal veins to dural venous sinuses and eventually to subdural and cerebral veins. Patients may present with seizures, hemiparesis, or nonspecific symptoms such as headache (70%), altered mental status, fever, and nausea and vomiting. Papilledema may be found on clinical exam if there is elevated intracranial pressure. Even with antibiotics, the mortality rate of brain abscess is 5–15%, reaching up to 80% if there is abscess rupture.
Imaging of sinusitis-associated complications
CT and MR contribute to the decrease of mortality of sinusitis-associated brain abscess by facilitating timely diagnosis, surgical drainage, and administration of antibiotics.
CT is useful in evaluating sinus disease and associated osseous findings such as sinus wall erosion or sclerosis.
Abnormal diffusion signal within the abscess cavity on DWI, bright T1 and dark T2 rim from free radicals in macrophages, and predominantly thin, smooth enhancement of the abscess wall differentiate abscess from other ring-enhancing lesions such as tumor or demyelinating disease.
Occasionally MR spectroscopy may be used to differentiate among causal organisms, with bacterial agents characterized by elevated amino acid (0.9 ppm) and lactate (1.3 ppm) peaks, fungal agents by trehalose (3.6; 3.8 ppm) peaks and toxoplasmosis and tuberculosis by lipid (1.3 ppm) peaks.
Treatment of sinusitis-associated complications
Treatment of sinusitis-associated brain abscess requires surgical drainage (for both diagnostic and therapeutic purposes) and antibiotics, often with concurrent sinus surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree