Diagnosis: Intracranial hypotension with subdural hematomas
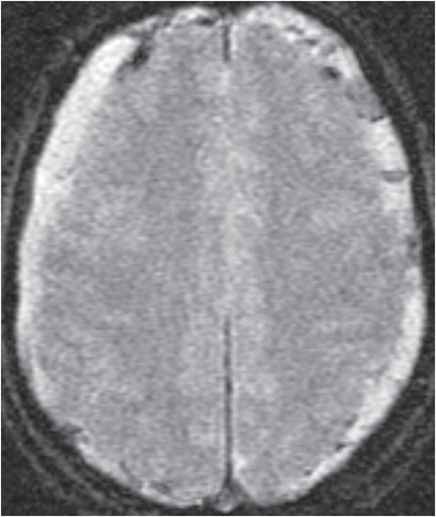
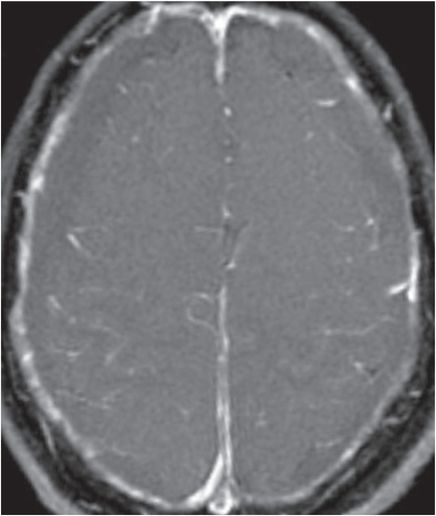
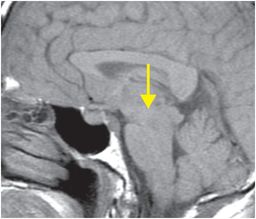
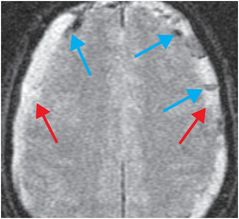
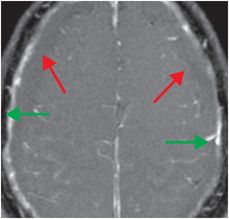
Sagittal T1-weighted image (left) shows downward sagging of the brainstem (yellow arrow). Axial gradient echo image (middle) shows bilateral subdural collections (red arrows) with areas of loculation and dark susceptibility effect (blue arrows) indicating blood products, consistent with chronic subdural hematomas. Gadolinium-enhanced axial T1-weighted image (right) reveals diffuse pachymeningeal thickening and enhancement (green arrows) with subjacent non-enhancing, intermediate intensity subdural collections (red arrows).
Discussion
Overview and physiology of intracranial hypotension
Intracranial hypotension is caused by iatrogenic or spontaneous cerebrospinal fluid (CSF) leak.
Clinical presentation includes orthostatic headache (worse in the upright position), dizziness, tinnitus, and abducens palsy. Headache may be absent.
When CSF volume is lost, intracranial volume is usually maintained by venous expansion. On imaging, this appears as pachymeningeal thickening and enhancement due to venous engorgement, with enlargement of the venous sinuses, pituitary gland, and cervical spine epidural plexus. Less frequently, cranial or spinal hygromas or hematomas form in the spinal or intracranial epidural or subdural spaces. Hematomas form as a consequence of tearing of subdural bridging veins. Loss of CSF volume results in loss of buoyant force, which results in brainstem sagging, descent of the cerebellar tonsils, downward tilt of the optic chiasm, and enlargement of the pituitary gland. Findings may be seen in isolation or combination.
Treatment of intracranial hypotension
Spontaneous CSF leaks can often be managed conservatively with bed rest, hydration, and caffeine or theophylline, but refractory cases may require epidural blood patch placement.
In the setting of intracranial hypotension, subdural hematomas are generally not evacuated due to risk of downward herniation and cerebellar hemorrhage. Instead, the cause of the CSF leak is addressed.
If an intraventricular shunt is present, the shunt pressure should be adjusted.
If there was recent spinal surgery, post-operative drains may need to be removed.
Clinical synopsis
This 62-year-old man with intracranial hypotension and chronic subdural hematomas was treated conservatively and made a full recovery.
Self-assessment
|
|
|
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








