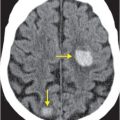
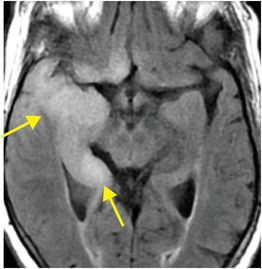
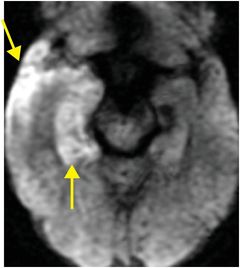
Diagnosis: Herpes simplex encephalitis
Axial FLAIR (left image) and T2-weighted (middle image) MR images show edema and swelling of the right temporal lobe (arrows) with minimal mass effect upon the cerebral peduncle. DWI (right image) reveals corresponding restricted diffusion.

Discussion
HSE is the most common cause of acute viral inflammation of the brain and meninges.
The clinical presentation of Herpes simplex encephalitis (HSV) typically involves deterioration of mental status, fever, headache, and seizures, often progressing over several days.
Other causes of viral encephalitis may have overlapping imaging and clinical manifestations and include Eastern Equine Encephalitis (EEE), influenza, and HIV. EEE is caused by an arbovirus infection, typically in late summer or autumn, with neurological deterioration progressing to coma within 1–3 days. HIV encephalitis is a chronic, indolent process that presents with cognitive decline.
Imaging findings of viral encephalitis
Whereas HSE typically involves one or both temporal lobes with putaminal sparing, EEE typically involves deep nuclear gray matter structures and the brainstem. HIV causes diffuse leukoencephalopathy. Influenza may involve the thalami, brainstem, and corpus callosum, but lobar and putaminal involvement is not typical. West Nile virus can produce various brain findings, but lacks a characteristic pattern.
CT is useful in uncooperative patients, as it can evaluate for other causes of mental status deterioration such as hemorrhage and tumor, and may show areas of brain swelling.
MRI is more accurate in characterizing sites and extent of brain involvement. Diffusion is often mildly restricted, but may be normal. Hemorrhage may accompany HSE, but is usually absent in EEE.
While MRI findings may suggest a specific etiology, diagnosis is established by serum or CSF analysis. Other processes involving the temporal lobe include tumor, middle cerebral artery territory stroke, and post-ictal change. Tumor has a more insidious onset than HSE. Tumor enhancement, if present, may aid in diagnosis. MR spectroscopy shows elevated choline in higher-grade neoplasms. Acute stroke presents with acute onset neurological symptoms, involves a vascular territory, and may involve the putamen. Post‐ictal change may be indistinguishable from HSE on imaging. This condition is characterized by restricted diffusion in the temporal lobe, which corresponds to depolarization and glutamate-mediated hyperexcitation.
Clinical management of viral encephalitis
When there is clinical suspicion for HSE, empiric antiviral treatment with acyclovir should begin immediately. The diagnosis may later be confirmed by CSF analysis, including Herpes simplex virus (HSV) polymerase chain reaction. Treatment for EEE is supportive, as no currently existing antiviral agent has been proven effective.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree