48 Vascular Diseases of the Hand and Fingers
Catheter-based angiography of the arteries in the arm and hand—an invasive procedure—is the method of choice for differentiating functional acral vasospasm of (primary) Raynaud disease from organic arterio-pathies. The most common causes of (secondary) Raynaud phenomenon are peripheral vascular disease (PVD, atherosclerosis), peripheral embolism, and endangiitis obliterans. Noninvasive MR angiography is well suited for visualization of the vessels for surgical planning the extent of vascular injuries, and malformations of the arteries and veins of the arm and hand. Color-coded Doppler ultrasonography (US) can display the perfusion of a vascular area, but its survey assessment is limited.
Diagnostic Imaging
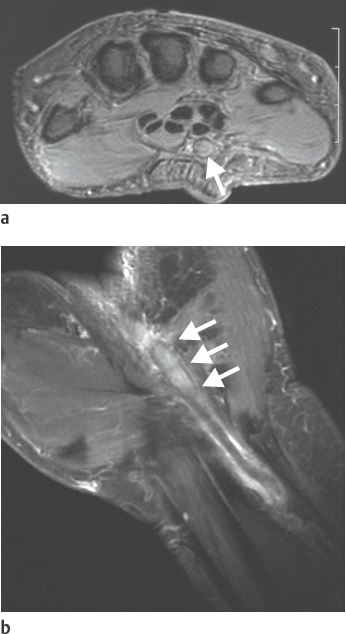
Instrumental evaluation of disturbances in acral circulation is largely achieved with noninvasive methods such as Doppler US, occlusion plethysmography, acral volume plethysmography, and capillary microscopy. Vessels can be directly visualized noninvasively with color-coded duplex US, which can identify the patency of arterial vessels up to the digital arteries. Angiographic examinations are performed to visualize morphological lesions such as stenoses, aneurysms, and arteriovenous malformations. MR angiography (MRA) offers a noninvasive method that is today preferred to arterial digital subtraction angiography (DSA) for workup of several vascular diseases. This is especially true for arteriopathies between the forearm and the metacarpus. However, MRA has only limited spatial resolution in the visualization of pathologically altered digital arteries.
Disease Entities
Peripheral Vascular Disease (Atherosclerosis)
Pathoanatomy and Clinical Symptoms
Atherosclerosis, a degenerative systemic disease of the arteries causing stenoses and occlusions, leads frequently to occlusions of peripheral arteries in the lower extremities. In the upper extremities, clinically manifest atherosclerosis is relatively rare. The main predisposed sites for vascular occlusion and stenoses are the supra-aortal arteries near their origins. Proximal stenoses and occlusions of the subclavian artery are more likely to cause vertebrobasilar than brachial symptoms.
Findings in DSA and MRA
If there is clinical suspicion of a peripheral vascular occlusion in the upper extremities, depiction of the entire aortic arch should always be obtained for reliable survey assessment. A special entity of occlusive arterial disease is the subclaviansteal phenomenon, which describes a reverse flow in one vertebral artery when there is a proximal stenosis or occlusion of the subclavian artery. Besides vertebrobasilar insufficiency, this type of occlusion can also lead to stress-induced claudication of the affected limb, which appears especially when one works with raised arms.
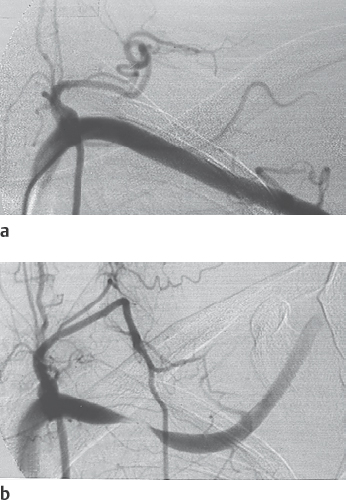
Vascular occlusions along the further course of the axillary and brachial arteries are relatively rare. With increasing age, elongation of the vessels in the forearm (which is not considered pathologic) can develop up to the digital arteries. Peripheral vascular stenoses rarely cause symptoms, and vascular occlusions are usually well compensated by tortuous collateral vessels ( Fig. 48.1 ). Critical circulatory conditions are often found in patients with terminal renal failure, in this case due to degenerative vascular alterations with calcification of the vessel walls. Arteriovenous shunt procedures can also be followed by peripheral vascular occlusions.
Peripheral Embolism
Pathoanatomy and Clinical Symptoms
Obstruction of a peripheral artery by an embolus leads to acute ischemia with a typical clinical appearance. Only about 6% of all arterial emboli occur in the upper extremities, and usually the axillary or brachial arteries are involved. The location of the occlusion can be determined clinically and with Doppler US with relative certainty. Catheter-based angiography is generally indicated for planning therapy and revealing the source of the embolus. Diagnostic difficulties can arise in chronic recurring small emboli, which can lead to the clinical appearance of Raynaud’s phenomenon. Only emboli in large vessels should be removed surgically with embolectomy, whereas the occlusions in the peripheral arteries can be treated with radiologic interventional methods (extraction and fragmentation approaches as well as local thrombolytic therapy). The special form of peripheral vascular occlusion caused by cyroglobulinemia should also be considered in differential diagnosis.
Findings in DSA and MRA
Angiographic signs of peripheral embolism are the abrupt interruption of the contrast-filled vessel with sharp contours at the site of occlusion and the lack of collateral vessels ( Figs. 48.3 – 48.5 ). The tip of the embolus in large vessels is delineated by the contrast agent and forms a dome (“dome sign”). This is more difficult to recognize in small digital arteries.
The subclavian artery is the second-most-common anatomic source of emboli after the heart chambers. One must consider the different forms of the thoracic-outlet syndrome with thrombogenic alterations of the vessel walls as the source of an embolus. Angiographic imaging including the subclavian artery must be performed in the functional position (with elevation of the upper arm) in some cases ( Fig. 48.2 ).



Endangiitis Obliterans (Winiwarter-Buerger Disease)
Pathoanatomy and Clinical Symptoms
Endangiitis obliterans (synonym: thrombangiitis obliterans) is an inflammatory vascular disease with a predilection for the small and middle-sized arteries and veins in the extremities. Progressive ischemia of the fingers or toes develops and can lead to soft-tissue necrosis in some cases. The upper extremities are more often affected. The symptoms are usually bilateral, although unilateral involvement has been observed. Men between 20 and 40 years of age are most commonly affected. The etiology is unclear, but nicotine abuse certainly plays a key role in the pathogenesis.
Findings in DSA and MRA
Endangiitis obliterans rarely affects the proximal arteries. For diagnostic evaluation, angiography of the brachial artery is sufficient. In catheter-based arteriography, functional pharmacoangiography should be performed using intra-arterially administered vasodilators such as acetylcholine chloride or glycerol trinitrate. MR angiography is of only limited diagnostic value in the assessment of the digital arteries because of its limited spatial and temporal resolution. Classification of endangiitis obliterans can be reliably achieved in advanced stages because of a characteristic pattern of vascular occlusion with a bizarre net work of collateral vessels. In contrast to other diseases, the corkscrew-shaped collaterals develop in the direct course of the occluded vessel ( Fig. 48.6 , Table 48.1 ). Angiographic differential diagnosis is challenging in early stages of endangiitis obliterans. Differentiation from Raynaud phenomenon caused by other underlying diseases can be unsuccessful.
Raynaud Disease
Pathoanatomy and Clinical Symptoms
The primary form (Raynaud phenomenon) describes an episodic vasospastic disturbance in acral circulation that can be triggered by cold or emotional stress. In primary Raynaud phenomenon, there is neither gangrene nor a recognizable underlying disease entity. This disease, which is of unknown etiology, affects women between puberty and 30 years of age in 90% of cases.

Findings in DSA and MRA
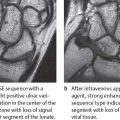
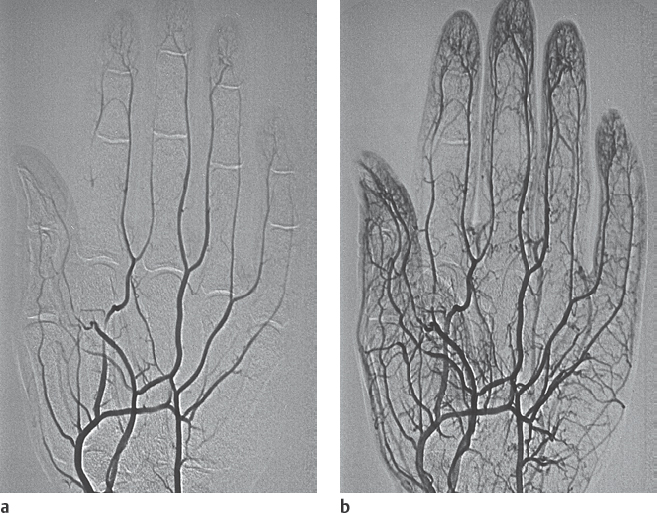
The arteries display extreme luminal narrowing with delayed arrival of the contrast agent into the vascular periphery. During pharmacoangiography, preferably with intra-arterial administration of a vasodilative substance, the vasospasm can be interrupted. This demonstrates reliable exclusion of organic vascular occlusions ( Fig. 48.7 ). Evidence of occluded digital arteries indicates secondary Raynaud disease. Conversely, in what appears to be primary Raynaud phenomenon, the underlying disease can become manifest as the disease progresses. Primary Raynaud phenomenon is actually only a diagnosis of exclusion. The underlying causes of secondary Raynaud disease are numerous and are listed in Chapter 62. Diagnostic differentiation of the primary form by angiographic evaluation is often impossible.
Collagenoses and Rheumatoid Arthritis
Scleroderma (Progressive Systemic Sclerosis)
Pathoanatomy and Clinical Symptoms
Scleroderma, a chronic disease of the connective tissue and blood vessels, displays Raynaud disease as an early leading symptom in 80% of cases. A disturbance in acral circulation of the hands can be the first and only symptom. The cause of this disease is unknown. Proliferation of the endothelial cells leads to an obliterative vasculopathy of the small arteries and capillaries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree