5 Chest
Approach and Analysis
Plain chest radiographs (chest X-rays, CXR) make up the bulk of imaging work in the emergency department. They are requested for virtually any suspected thoracic disease, to exclude (or detect) active tuberculosis in patients who will be admitted to hospital psychiatry units or to public shelters, and for screening in patients who will have urgent surgery. CT is reserved for patients with acute chest pain, hypoxia, and dyspnea in whom the chest radiograph does not provide a satisfactory diagnosis. The most common indications for CT are for investigation of possible pulmonary embolism, aortic dissection, and traumatic injury.
Anatomic Checklist
Radiographs
Tubes and lines
Trachea
Heart
Mediastinum and hila
Central pulmonary vessels
Lung parenchyma (including peripheral 1 cm)
Bones
Soft tissues
Computed Tomography
Lower cervical soft tissues
Trachea and airways
Mediastinum and hila
Aorta
Pulmonary Arteries and Veins
Carotid, vertebral, and subclavian arteries
Jugular, brachiocephalic veins, and superior vena cava
Heart, Coronary Arteries, and Pericardium
Lungs
Chest wall and diaphragm
Upper abdomen
Imaging and Anatomy
Radiography
Posteroanterior (PA) radiographs are obtained in full inspiration with the patient′s chest against the detector and the arms positioned to rotate the scapulae away from the lungs. Anteroposterior (AP) portable radiographs, on the other hand, are obtained with the detector cassette behind the patient, the X-ray source about 6 ft (2 m) in front, the arms at the patient′s sides, and the scapulae superimposed on the upper lungs. On AP radiographs the normal divergence of the X-ray beam and the increased distance between anterior thoracic structures and the detector leads to arti-factual magnification of the cardiomediastinal silhouette and indistinct pulmonary vessels, particularly in larger patients. By contrast, because the X-ray source is behind the patient for PA radiographs, arti-factual magnification of the heart is of less concern than on AP radiographs. Moreover, because the cassette for AP radiographs is against the patient′s back, sometimes the skin can fold on itself against the cassette and produce a line similar to that seen with pneumothorax; this does not occur with PA radiographs. For these reasons, unless the patient cannot tolerate a PA radiograph, it is always preferred to a portable AP study.
Lateral radiographs are usually obtained with the right chest against the detector and the arms above or in front of the patient. The right hemidiaphragm appears continuous from front to back. The left hemidiaphragm blends into the cardiac shadow. Except for the rare patient with situs inversus, the gastric air bubble should be located immediately below the left hemidiaphragm.
Computed Tomography
Trauma
Indications: Chest trauma (usually performed in conjunction with abdominal CT)
Arterial phase: bolus track to aorta 150 HU
Oral contrast: None
IV contrast: 1.5 mL/kg at 4 mL/sec, followed by 20 mL saline at 4 mL/sec
Images: 5-mm axial with 0.625-mm reconstruction and 1.25-mm coronal and sagittal reformations
Approximate radiation dose: 1,200 mGy
“Routine”
Indications: Evaluation of plain radiographic abnormalities, pulmonary nodules and masses, empyema
IV contrast (optional): 1.5 mL/kg at 4 mL/sec, 40-second delay
Images: 5-mm axial with 0.625-mm reconstruction and 1.25-mm coronal and sagittal reformations
Approximate radiation dose: 320 mGy
Pulmonary Embolism
Indications: Acute chest pain in setting of immobilization, hypercoagulable state, underlying malignancy, or other risk factors for pulmonary embolus
Pulmonary arterial phase: bolus track to main pulmonary artery 150 HU
IV contrast: 1.5 mL/kg at 4 mL/sec, followed by 20 mL saline at 4 mL/sec
Images: 5-mm axial with 0.625-mm reconstruction and 1.25-mm coronal and sagittal reformations
Approximate radiation dose: 650 mGy
Aortic Dissection
Indications: Acute chest pain in setting of hypertension, connective tissue disorder, or other risk factors for arterial dissection or aortic rupture
Arterial phase: bolus track to aorta 150 HU
IV contrast: 1.5 mL/kg at 4 mL/sec, followed by 50 mL saline at 4 mL/sec
Images: 5-mm axial with 0.625-mm reconstruction and 1.25-mm coronal and sagittal reformations
Approximate radiation dose: 1,000 mGy
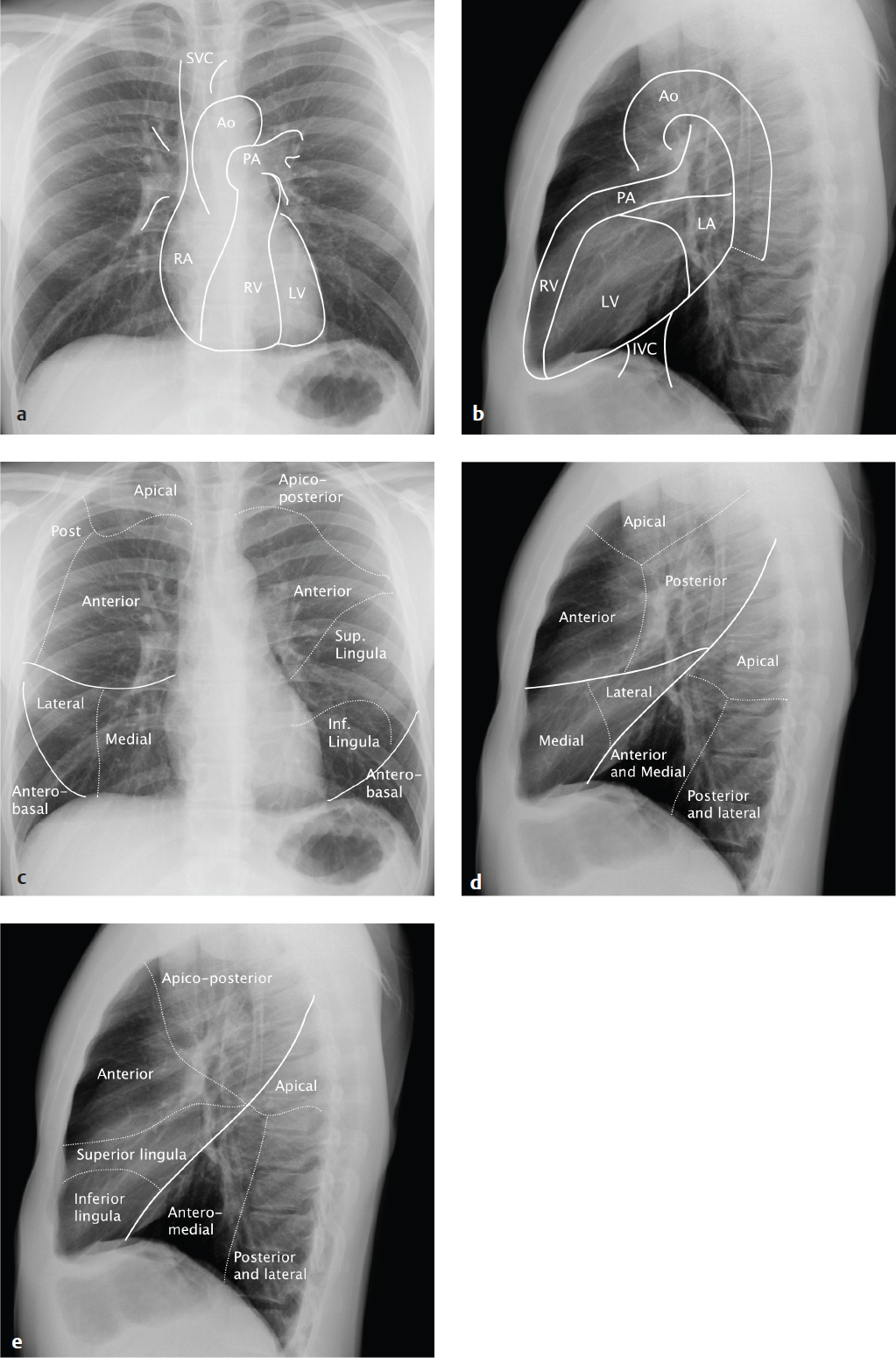
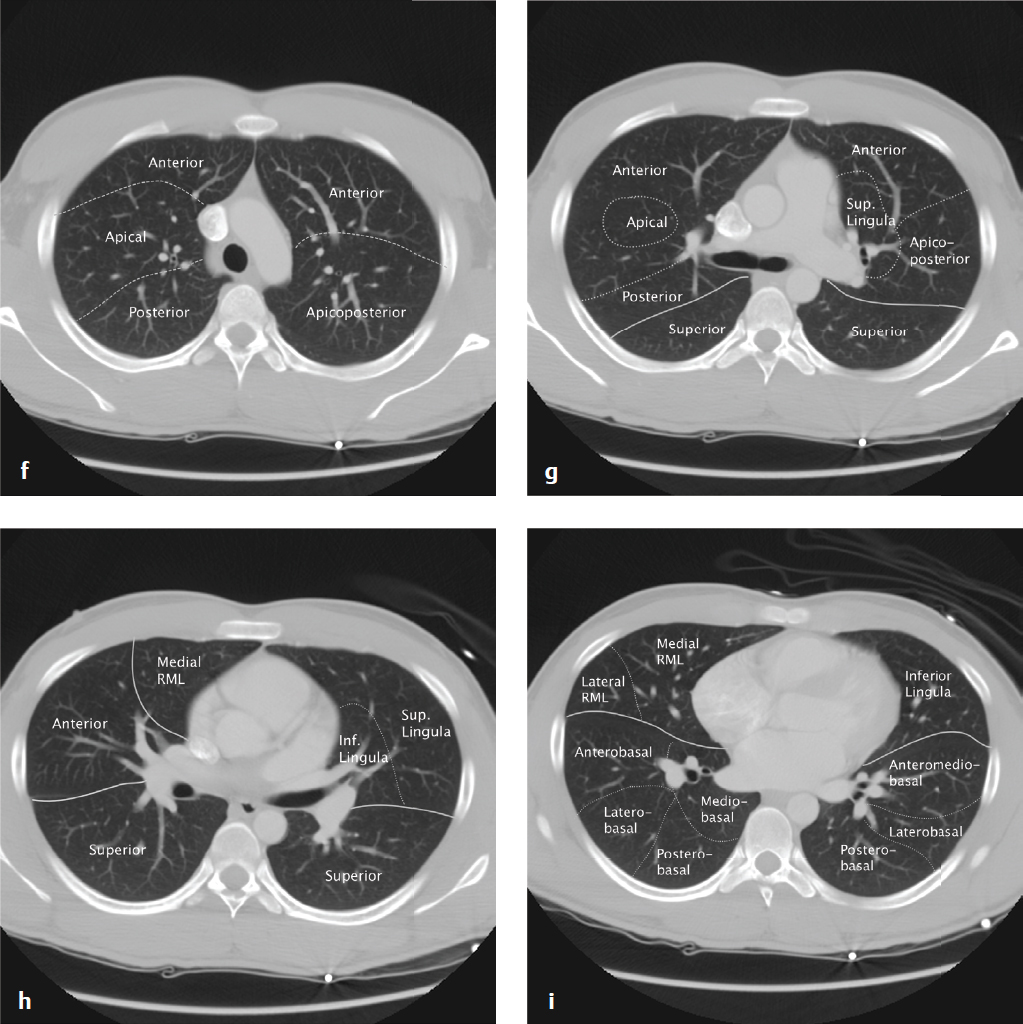
Anatomy
Knowledge of pulmonary segmental anatomy on radiographs and CT is necessary for accurate localization and description of pulmonary lesions ( Fig. 5.1 ).
Clinical Presentations and Differential Diagnosis
Clinical Presentations and Appropriate Initial Studies
Trauma
CXR
CT with contrast (arterial phase)
Echocardiography to evaluate pericardial effusion and cardiac function
– Aortic or other vascular injury
– Hemothorax
– Cardiac rupture
– Hemopericardium
– Pneumothorax
– Pneumomediastinum
– Pulmonary contusion or laceration
– Aspiration
– Rib fractures (flail chest)
– Diaphragm injury
– Sternal fracture
– Clavicle dislocation
– Spine fracture or dislocation
Dyspnea
CXR
CT without contrast may be useful for further evaluating radiographic findings
CT angiogram for exclusion of pulmonary embolism
– Pneumothorax
– Pleural effusion
– Pneumonia
– Aspiration
– Reactive airways disease
– Inhalational disease
– Cardiogenic pulmonary edema
– Noncardiogenic pulmonary edema
– Acute respiratory distress syndrome
– Pulmonary embolism
– Radiation pneumonitis (1–4 months posttreatment)
– Drug reaction
Chest Pain
CXR
Echocardiography to evaluate pericardial effusion and cardiac function
CT angiogram for exclusion of pulmonary embolism
CT angiogram for exclusion of aortic dissection or rupture
Coronary CTA may be useful for assessing myocardial infarction risk in selected patients
– Pneumonia
– Pulmonary embolism/infarct
– Myocardial ischemia
– Aortic dissection or rupture
– Pneumothorax
– Pneumomediastinum
– Neoplasm
Cough/Fever
CXR
CT without contrast may be useful for further evaluating radiographic findings
– Pneumonia
– Empyema
– Septic pulmonary emboli
Differential Diagnosis
Pneumomediastinum
Penetrating trauma
Barotrauma (vomiting, Valsalva, asthma)
Aspirated foreign body
Esophageal tear
Subdiaphragmatic free air
Anterior Mediastinal Mass
Lymphoma
Thymoma
Substernal goiter
Germ cell tumor
Middle Mediastinal Mass
Lymphadenopathy
Bronchogenic cyst
Aortic or pulmonary artery aneurysm
Posterior Mediastinal Mass
Neurogenic tumor
Lymphoma
Neurenteric cyst
Hilar Adenopathy
Lymphoma
Sarcoidosis
Infection
Metastatic disease
Pulmonary Edema
Cardiogenic
Fluid overload
Head injury
Acute respiratory distress syndrome (ARDS)
Inhalational injury
Transfusion reaction
Drug-induced
High altitude
Septal Lines/Interstitial Edema
Left ventricular (LV) failure
Mitral stenosis
Pulmonary veno-occlusive disease
Interstitial lung disease
Lymphangitic carcinomatosis
Air Space Opacification
Pulmonary edema
Pneumonia
Hemorrhage
Adenocarcinoma (bronchioloalveolar cell)
Sarcoidosis
Lobar Pneumonia
Streptococcus pneumoniae
Klebsiella pneumoniae
Staphylococcus aureus
Tuberculosis (primary)
Parenchymal Disease in HIV
Pneumocystis pneumonia
Tuberculosis
Fungal infection
Kaposi sarcoma
Interstitial Disease—Upper Lobe
Tuberculosis
Sarcoidosis
Cystic fibrosis
Interstitial Disease—Lower Lobe
Idiopathic pulmonary fibrosis
Scleroderma
Chronic aspiration
Asbestos-related disease
Bronchiectasis
Remote infection
Cystic fibrosis
Immunodeficiency
Allergic bronchopulmonary aspergillosis
Solitary Pulmonary Nodule
Granuloma (tuberculosis, histoplasmosis, coccidioidomycosis, cryptococcosis)
Bronchogenic carcinoma
Metastasis
Adenocarcinoma
Hamartoma
Arteriovenous malformation
Multiple Pulmonary Nodules
Metastases
Septic emboli
Granulomatous disease
Rheumatoid arthritis
Sarcoidosis
Miliary Nodules
Tuberculosis
Metastases
Fungal disease
Remote varicella pneumonia
Cavitary Nodules/Masses
Tuberculosis
Primary lung carcinoma
Metastases (especially squamous cell carcinoma)
Infected bulla
Wegener granulomatosis
Rheumatoid arthritis
Septic emboli
Ground Glass Opacification (CT)
Cardiogenic pulmonary edema
Acute respiratory distress syndrome (ARDS)
Atypical pneumonia
Pulmonary hemorrhage
Perilymphatic Nodules (CT)
Sarcoidosis
Lymphangitic carcinomatosis
Pneumoconiosis
Centrilobular Nodules (CT)
Infectious bronchiolitis (Mycobacterium avium intracellulare, tuberculosis)
Hypersensitivity pneumonitis
Endobronchial tumor
Respiratory bronchiolitis interstitial lung disease (RB-ILD)
Pneumoconiosis
Pleural Effusion
Trauma (hemothorax)
Viral pleuritis (usually with otherwise normal chest radiograph)
Congestive heart failure
Hepatic failure
Parapneumonic effusion
Neoplastic effusion
Pulmonary infarct
Subphrenic abscess
Pleural Based Mass
Metastasis
Empyema
Mesothelioma
Fibrous tumor of pleura
Pneumothorax
Spontaneous
Iatrogenic
Trauma
Secondary to lung disease
Secondary to pneumomediastinum or pneumoperitoneum
Chest Wall Injuries
Sternal fractures are a marker of high-energy impact and are seen in approximately 8% of patients with blunt thoracic trauma. Retrosternal hematoma, myocardial contusion, coronary artery tear, aortic laceration, and tracheobronchial tear are potential associated injuries.
Sternal fractures are not visible on supine portable AP chest radiographs, but they can be detected with a true lateral view. In practice, they are usually diagnosed on CT and are most commonly located 2 cm below the sternomanubrial joint. Retrosternal hematoma may be the consequence of great vessel injury or hemorrhage from small vessels; identification of normal fat between a substernal hematoma and the aorta indicates that the hematoma is not due to aortic rupture.
Sternoclavicular dislocation consists of anterior or posterior displacement of the medial clavicle relative to the sternal manubrium. Posterior dislocation, in which the clavicular head is located dorsal to the manubrium, typically results from a blow to the dorsal shoulder or to the anteromedial clavicle and can be associated with serious morbidity; as the medial clavicular head is driven into the soft tissues of the thoracic inlet, it can impact or injure the trachea, esophagus, recurrent laryngeal nerve, or great vessels. Anterior dislocation, resulting from a frontal blow to the ipsilateral shoulder, is more common and carries less risk of associated injury.
The sternoclavicular joint is difficult to assess on plain radiographs. CT permits accurate characterization of the dislocation and any hematoma or vascular impingement. Sternal dislocations are usually treated by closed reduction in the absence of associated mediastinal injuries.
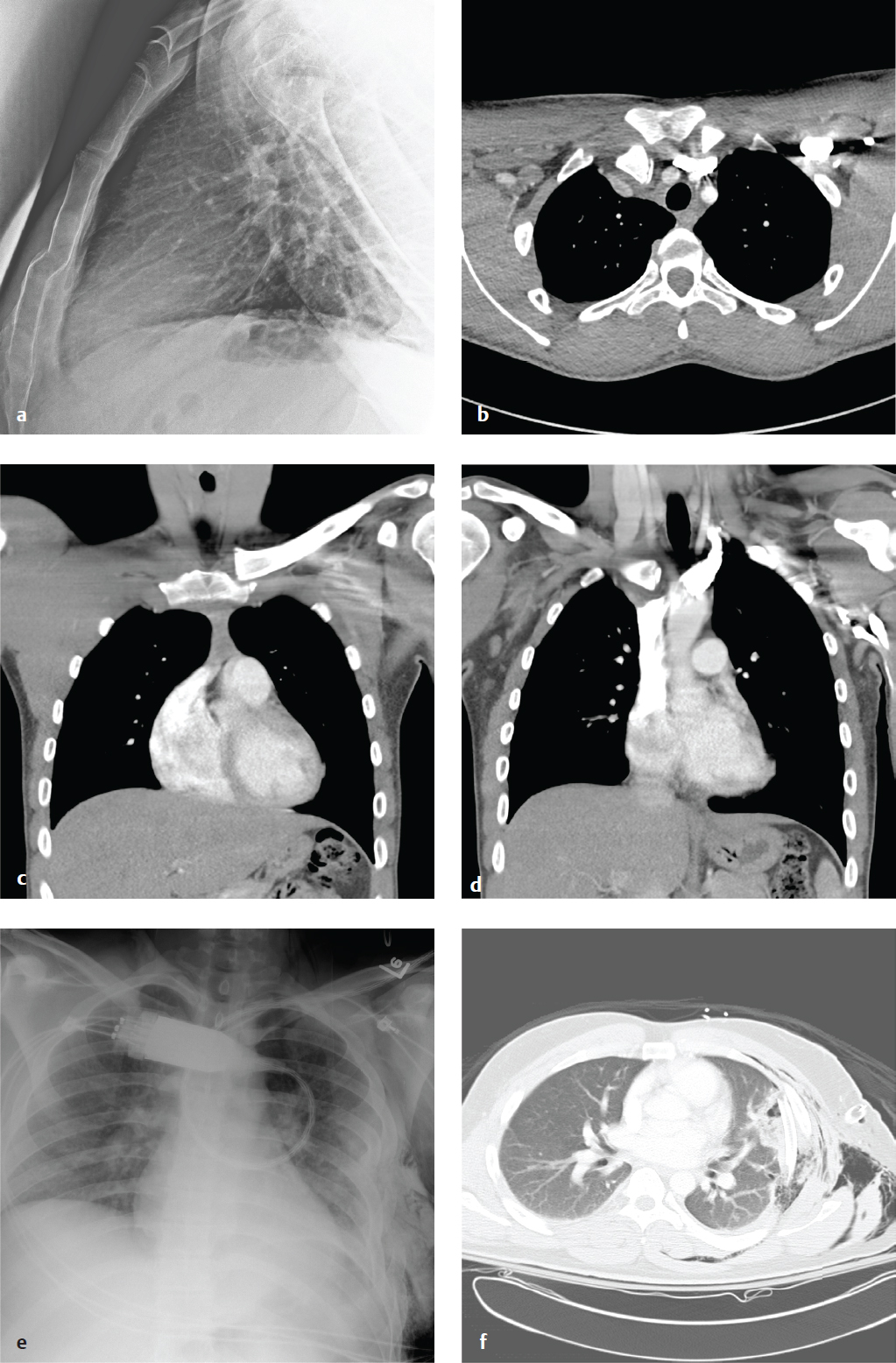
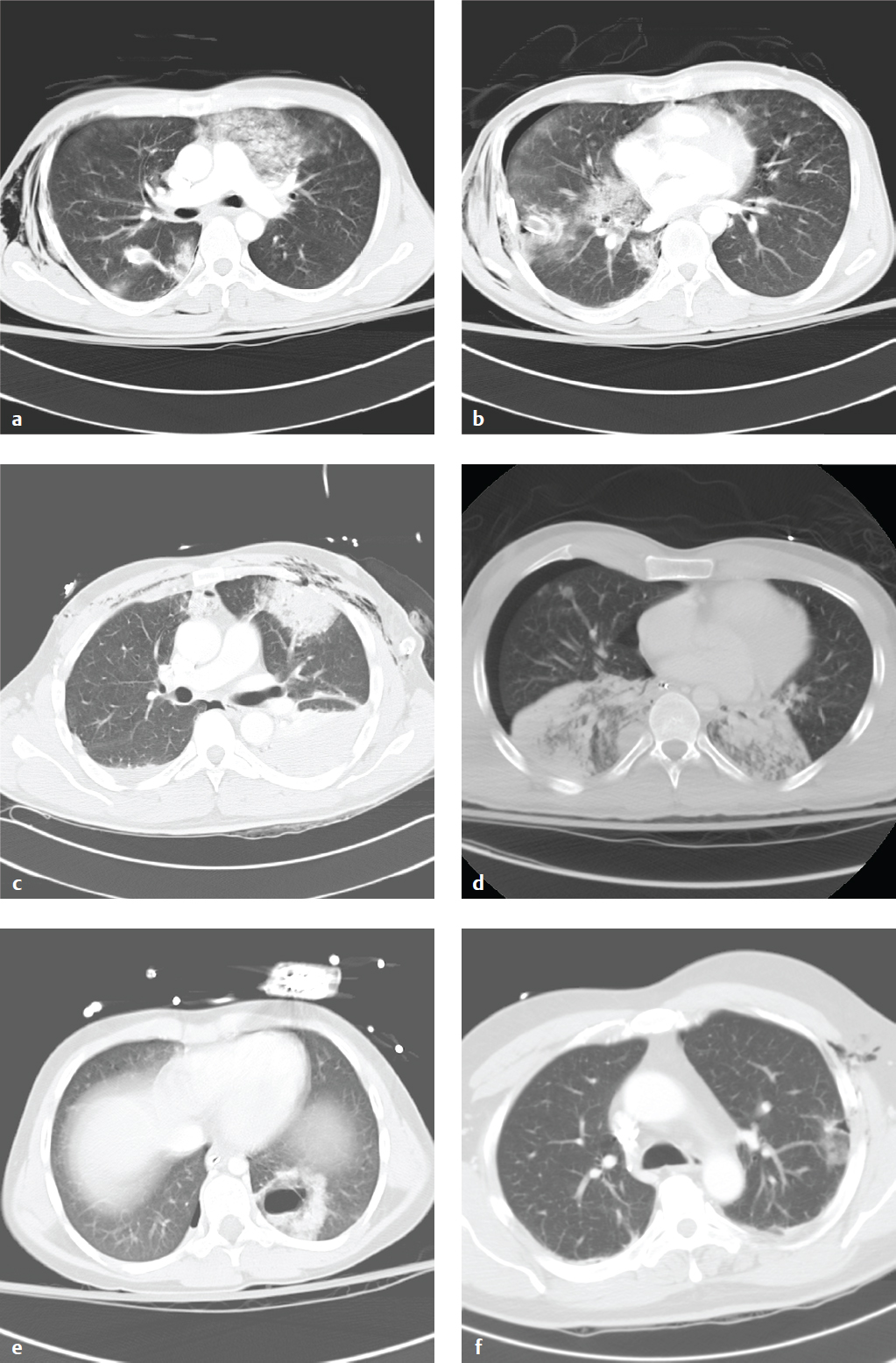
The term flail chest refers to thoracic injury with five or more adjacent simple rib fractures or more than three segmental rib fractures; it can lead to impaired ventilation and respiratory failure in the trauma patient. The normal thorax increases in volume on inspiration. In flail chest, the affected side, lacking structural support, retracts inward under negative intrapleural pressure as the diaphragm contracts. On expiration, positive intrapleural pressure allows the free-floating segment of fractured ribs to bulge outward, referred to as paradoxical respiration. Flail chest is extremely painful, and patients display rapid shallow breathing. Hypoxia is usually a consequence of associated pulmonary contusion rather than simple hypoventilation. Management includes supplemental oxygen and analgesics and may require regional nerve blocks or epidural anesthesia in severe cases ( Fig. 5.2 ).
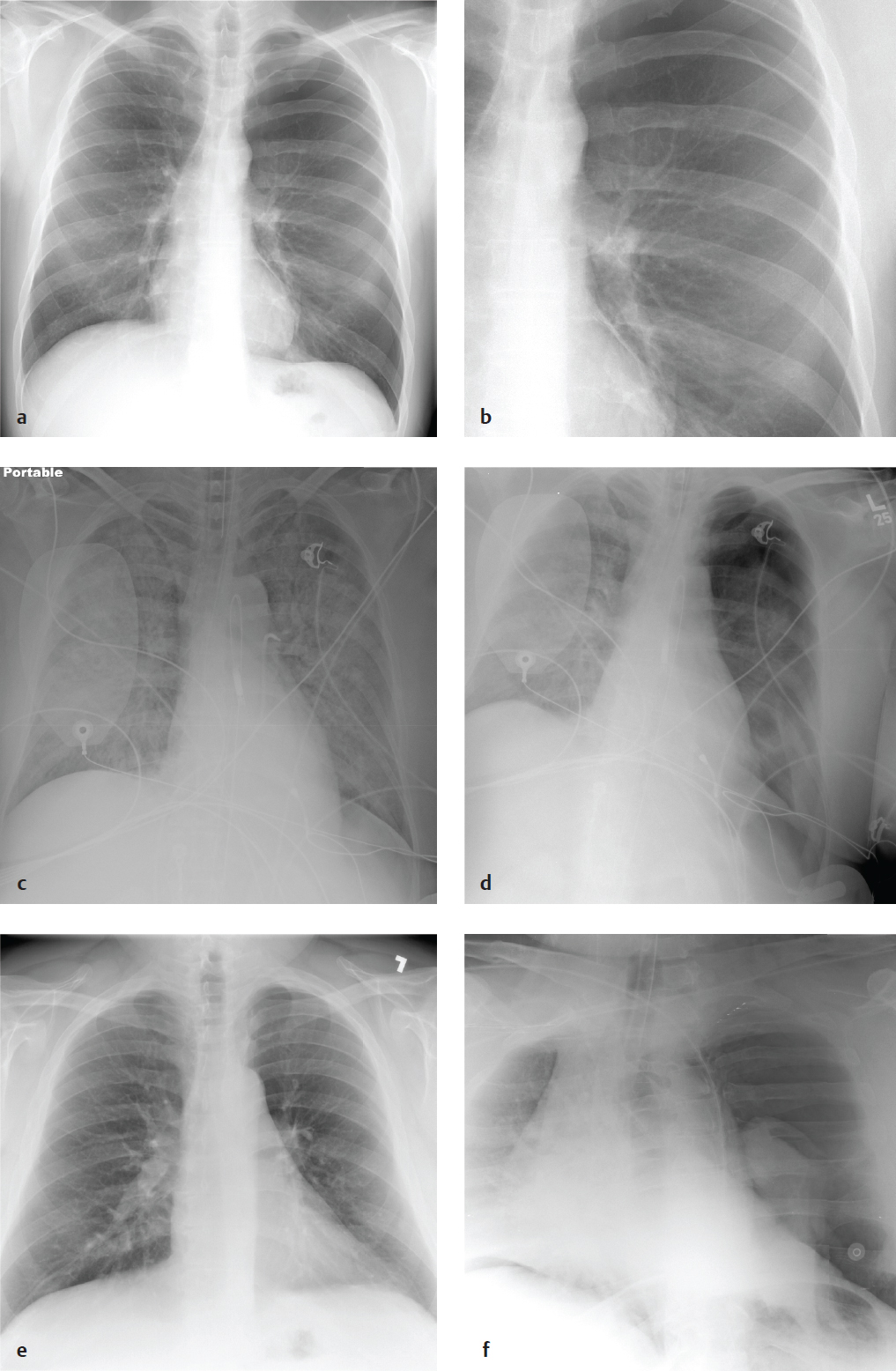
Pneumothorax
Pneumothorax is the intrapleural accumulation of air due to a visceral pleural tear. It can be caused by barotrauma, rupture of a peripheral bleb or other pulmonary lesion, and blunt or penetrating chest trauma. Especially in traumatic pneumothorax, a oneway valve effect allows air to accumulate on inspiration that cannot exit the pleural space on expiration. As intrapleural pressure on the side of the pneumothorax exceeds atmospheric and contralateral intrathoracic pressure, the trapped air displaces and compresses the mediastinum, reducing cardiac output and systemic perfusion. Clinical signs include diminished breath sounds over the affected hemithorax, tachycardia hypotension, jugular venous distention, and contralateral tracheal shift.
Smoking is the most common risk factor for spontaneous pneumothorax, which is usually due to rupture of a subpleural bulla. Primary pneumothorax typically occurs in persons under the age of 35 and is not associated with lung disease. Secondary pneumothorax is associated with underlying lung disease, such as chronic obstructive pulmonary disease, asthma, cystic fibrosis, interstitial lung disease, and malignancy. Patients typically present with acute pleuritic chest pain and dyspnea, but many are only minimally symptomatic.
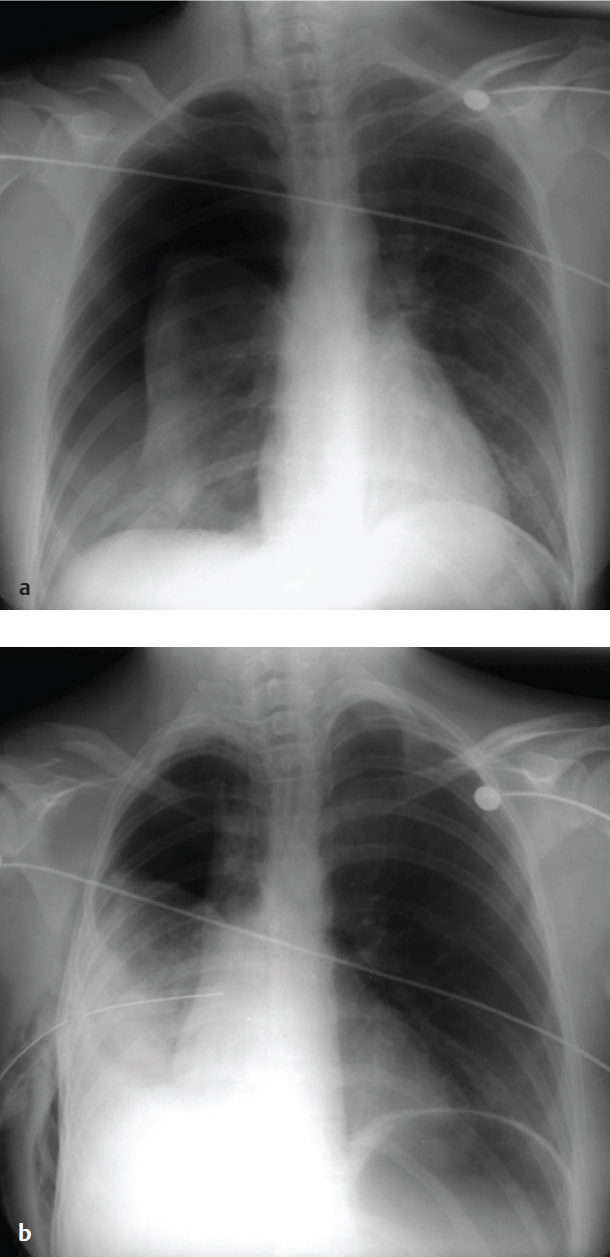
On upright PA radiographs, a fine, dense line that corresponds to the visceral pleura separates the lucent, air-filled lung from within the enlarged pleural space. Pulmonary vessels and other lung markings are not visible lateral to the visceral-pleural line. The heart and mediastinum are often normal in position but may be displaced to the opposite side in tension pneumothorax.
Supine, portable radiographs obtained in trauma patients often do not show pneumothoraces even when present, partly because air in the pleural space lies anterior, rather than lateral to the lung and the pleura is imaged en face rather than tangentially. Thoracic hyperlucency that extends over the upper abdomen is referred to as the “deep sulcus” sign and is a useful but indirect finding in acute trauma. Ultrasound can identify pneumothorax in the trauma setting, but findings are often subtle. Interrogation of the normal lung shows mobile dotlike echoes as the visceral pleura moves against the parietal pleura with respiration. In pneumothorax these mobile echoes are not seen.
Skin folds can simulate the appearance of a pneumothorax but are seen exclusively on portable AP chest radiographs. When the detecting plate is placed behind the patient, redundant skin can fold against the plate, causing an air–soft tissue interface external to the patient. A true pneumothorax will appear as a thin white line separating dark intrapleural air from dark air-filled lung. A skin fold (pseudopneumothorax) will appear as a dense edge against more lucent lung usually containing visible peripheral vessels.
In patients with hypoxia or vascular collapse, treatment should not be delayed while awaiting chest radiograph. A 14–16 gauge intravenous catheter can be inserted, either in the second anterior intercostal space in the midclavicular line or in the fifth intercostal space on the anterior axillary line, before a larger chest tube can be placed ( Fig. 5.3 ).
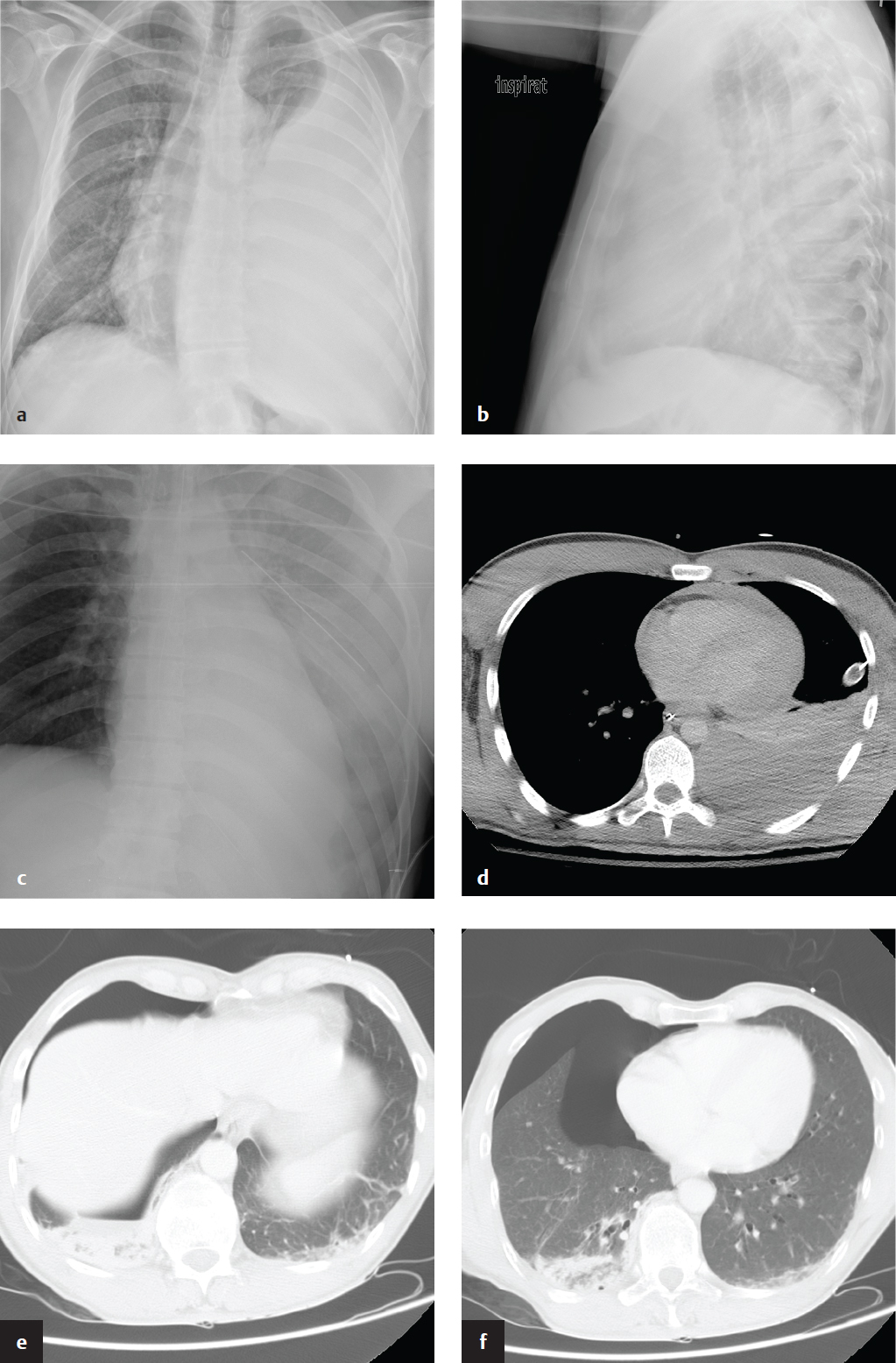
Hemothorax
Injury to the chest wall, lung parenchyma, diaphragm, heart, or great vessels can result in intrapleural hemorrhage, most commonly from intercostal or internal mammary artery disruption. Hemothorax due to pulmonary parenchymal injury from stabbing or contusion is often small and self-limited because of the low pulmonary vascular pressure and usually subsides spontaneously or following placement of a pleural drain.
Massive hemothorax (> 1 liter) with clinical signs of shock and hypoperfusion is a surgical emergency due to potential heart and great vessel tamponade from the accumulated blood, acute hypovolemic shock, and hypoxia from lung collapse.
Supine chest radiographic findings are often subtle, depending on the volume of blood. Hazy increased density of the involved hemithorax with preserved vessel definition may be seen in smaller posterior hemothoraces. Large amounts of blood can fill the pleural space lateral to the lung and appear as a dense crescent-shaped collection. CT with arterial-phase contrast enhancement is diagnostic; acute blood products have an attenuation of 35–70 HU, and layering of intrapleural fluid with different densities due to combinations of clot, blood cells, and serum can be seen. In addition, CT optimally evaluates the integrity of the great vessels and identifies areas of arterial extravasation and other associated injuries.
Initial management is by placement of a chest tube, which permits evacuation of clot, reexpansion of the collapsed lung, and effective tamponade of low-pressure bleeding. Definitive surgical management depends on the nature of the injury and source of hemorrhage ( Fig. 5.4 ).
Pulmonary Contusion and Laceration
Pulmonary contusion is a complication of blunt chest trauma and reflects focal parenchymal injury, edema, and interstitial and alveolar hemorrhage. Chest radiographic findings range from irregular nodular opacities to large areas of consolidation, but plain films are often nonspecific; aspiration pneumonitis can have a similar appearance and can also be seen in the trauma setting. On CT, pulmonary contusions appear as focal peripheral lung opacification adjacent to an area of impact. Posterior and lower lobes are more commonly affected. In contrast to lobar pneumonia, pulmonary contusions do not respect fissures and do not localize to a segment. They may be widespread, simulating ARDS or alveolar edema. In most cases, pulmonary contusion is apparent on the initial examination and does not worsen in severity. Radiographic clearing is rapid, and pulmonary contusions can resolve in as few as 72 hours.
Pulmonary laceration consists of a traumatic parenchymal disruption with subsequent formation of a hematoma or air-filled cavity (pneumatocele). The injury is typically due to shearing forces and is seen in blunt and penetrating injury. Lacerations are often obscured by concomitant pulmonary contusion, hemothorax, or pneumothorax and are easily missed on portable chest radiographs. Nearly all acute lacerations are detected with CT and appear as discrete round or oval air or fluid collections within an area of surrounding consolidation.
There are four types of pulmonary laceration. Type 1 (compression rupture injury) is most common and due to sudden compression of the chest wall with rupture of the inflated lung parenchyma. Type 2 (compression shear injury) results from compression of the lower chest with displacement of the lower lobe across the spine, causing a paravertebral cavity. Type 3 (rib penetration tear) is a small peripheral laceration adjacent to a rib fracture. Type 4 (adhesion tear) is the result of a preexisting pleuropulmonary scar ( Fig. 5.5 ).
Tracheobronchial Rupture
Tracheobronchial rupture is rarely encountered in clinical practice because most patients with this injury die from respiratory failure or exsanguination before arriving at the emergency department. Abrupt deceleration and intrathoracic shearing forces as well as compression of the airways between the sternum and thoracic spine in blunt trauma can disrupt the trachea or mainstem bronchus. Most injuries occur within 2.5 cm of the carina.
The most common imaging findings are pneumomediastinum and pneumothorax. Persistent pneumothorax after chest tube placement and suction is the hallmark of a major bronchial injury. With complete bronchial transection, the ipsilateral lung falls to the dependent (usually posterior) portion of the hemithorax; the “fallen lung” sign.
Chest CT can identify the exact site of the tear as a focal or a circumferential defect in the tracheal or bronchial wall. Other findings include airway wall contour deformity, extraluminal location of the endotracheal tube tip or herniation/overdistension of the balloon, pneumomediastinum, and deep cervical soft tissue emphysema ( Fig. 5.6 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree