5 The Pleura
Introduction
The pleura, derived from the Greek word for side, is the serous membrane that covers the lung parenchyma, mediastinum, diaphragm, and rib cage. The pleura allows the lung to expand and contract within the rigid confines of the thoracic cavity by transmitting mechanical forces from the diaphragm and chest wall with minimal friction. They also serve as a protective barrier from infection. 1
Embryology
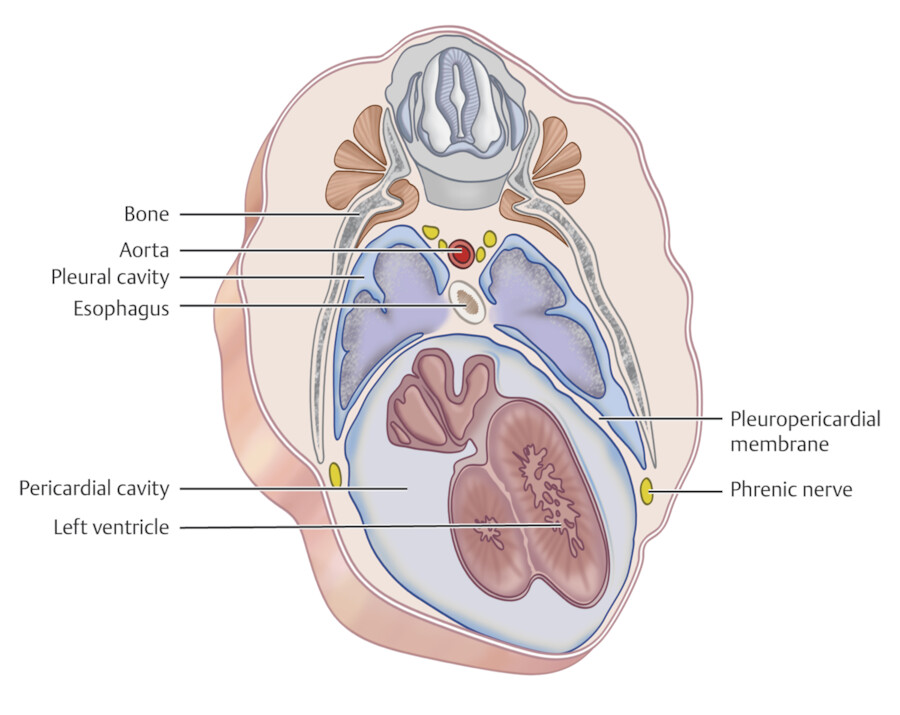
The cephalad portion of the embryonic coelomic cavity enlarges during week 4 of development, becoming the pericardial cavity and communicating on each side with the pleural canals. The pleural canals in turn communicate with the peritoneal canals. These compartments of the coelomic cavity are divided by three partitions: (1) the septum transversum serves as an early partial diaphragm, (2) the pleuropericardial membranes divide the pericardial and pleural cavities, and (3) the pleuroperitoneal membranes join with the septum transversum to complete the diaphragm which serves as the partition between each pleural cavity and the peritoneal cavity. The resulting pleural cavity is completely lined by a mesothelial membrane that develops from the somatic mesoderm to become the parietal pleura. The pleural cavity is complete by the third month. 1
The primordial bronchial buds are recognizable by 24 days and lie together with the trachea in a median mass of mesenchyme that is cranial and dorsal to the peritoneal cavity (Fig. 5‑1). This mesenchyme develops into the mediastinum and separates the pleural cavities. The lung buds bulge into the right and left pleural cavities, carrying with them a lining of mesothelium that develops from the splanchnic mesoderm to become the visceral pleura. As the separate lobes of the lung develop, their mesothelial covering is retained as the visceral pleura in the fissures. 1
The Pleura
The pleura is comprised of the parietal and visceral pleura. The parietal pleura measures 0.1 mm in thickness and is composed of a single layer of mesothelial cells joined with a layer of loose connective tissue containing systemic capillaries, lymphatic vessels, and sensory nerves. The parietal pleura lines the thoracic cavity and is separated from the endothoracic fascia, which lines the inner ribs and innermost intercostal muscles, by a layer of extrapleural fat along most of the chest wall (Fig. 5‑2) (see Chapter 1, Thoraic Wall). This extrapleural fat is continuous with the mediastinal fat, therefore mediastinal processes including air, inflammation, or edema can infiltrate into the extrapleural space. The parietal pleura is subdivided by the surfaces it covers into the mediastinal, costal, and diaphragmatic parietal pleura (Fig. 5‑3, Fig. 5‑4). It is strongly adherent to the fibrous pericardium and diaphragm. 2 , 3
The visceral pleura measures 0.1 to 0.2 mm in thickness and consists of single layer of mesothelial cells that joins with the fibroelastic fascia of the subpleural interstitium of the lung. It adheres to the lung parenchyma from the hilum outward and lines the interlobar fissures. 2 , 3 The closed potential space between the parietal and visceral pleura is known as the pleural space. It typically contains a thin film of fluid that acts as lubricant to minimize friction as the visceral pleura slides along the parietal pleura during respiration. Many disease processes can lead to fluid accumulation in the pleural space, known as a pleural effusion. The right and left pleural space are separated by the mediastinum and do not normally communicate. 1
The visceral pleura merges with mediastinal parietal pleura at pulmonary root and encloses the structures of the pulmonary hilum. At the inferior aspect of the root, the reflection of the mediastinal pleura over the visceral pleura continues as a bilayered sheet of both visceral and parietal pleura (total of four layers) in the front and back of the hilar plane to form the inferior pulmonary ligament (also known as the triangular ligament), that is carried downward and more posteriorly from the medial aspect of the lung to the mediastinum (Fig. 5‑5 , Fig. 5‑6). Medially, the inferior pulmonary ligament is inserted on the right side along the right lateral border of the esophagus and on the left side on the posterior aspect of the pericardium and thoracic aorta (Fig. 5‑5 , Fig. 5‑6 , Fig. 5‑7). The lower border is located posteriorly, has a variable configuration, and may insert on the diaphragm (Fig. 5‑7). The inferior pulmonary ligament contains loose connective tissue, bronchial and esophageal arterial branches, venules that empty into superior diaphragmatic veins, and lymphatic trunks and nodes that drain the lower lobes of the lung and lower third of the esophagus. 4 Blood vessels in the ligament could be the source of hemorrhage following blunt thoracic injuries. After trauma, air may dissect into the ligament and produce a localized pneumothorax or bleb. Inferior pulmonary ligament is usually seen as a linear or triangular structure at posterior cardiophrenic angles on axial CT images.
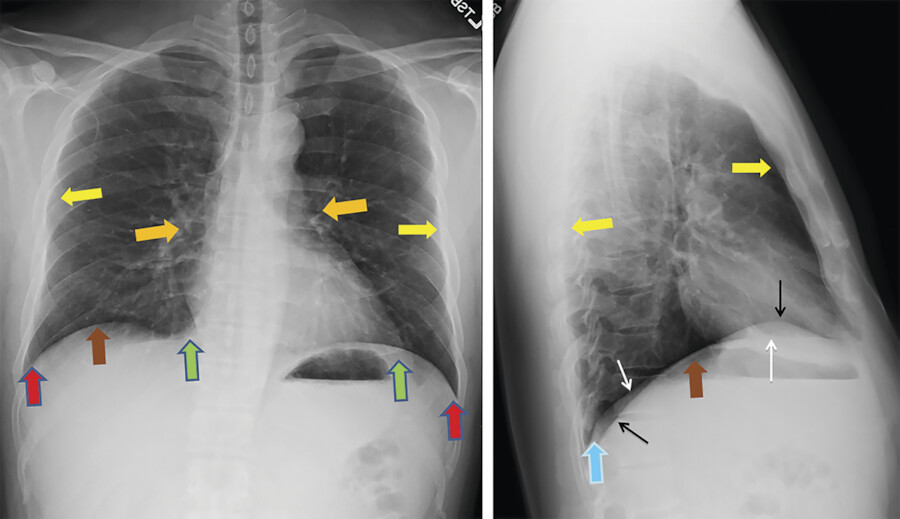
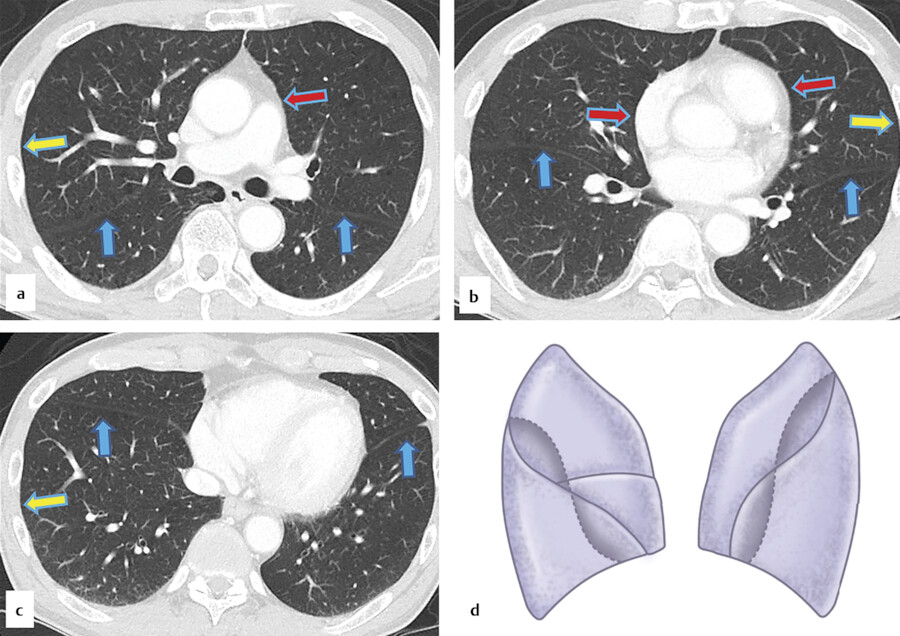
The interlobar fissures separate lobes of the lungs and extend from the hilum to the lung surface (Fig. 5‑4 , Fig. 5‑8). Normal major fissures consist of double layers of infolded invaginations of the visceral pleura. The oblique (major) fissures originate posteriorly near the T4–T5 level and terminate along the anterior diaphragmatic pleura. The right oblique fissure separates the right upper and middle lobes from the right lower lobe. The left oblique fissure separates the left upper and lower lobes. The right major fissure is shorter and wider than the left. The lower part of the left oblique fissure is more posterior due to anterior location of the heart in the left hemithorax. Both fissures have an undulating course with the upper part concave anteriorly and faces laterally, whereas the lower part is convex anteriorly and faces medially (Fig. 5‑4 , Fig. 5‑5). This configuration is variable. The right minor fissure separates the right middle and upper lobes. 1 , 2 , 3 Radiological identification of a lesion in relation to a fissure is important for precise localization of a lesion. Oblique fissures are best identified on lateral chest X-rays and the minor fissure on both lateral and frontal views (Fig. 5‑8). The superolateral part of oblique fissure can be identified on frontal X-rays as a curving contour, line, or edge at the upper lateral lung field due to small pleural fluid or extrapleural fat 5 (Fig. 5‑9). The superomedial part of the oblique fissure may also be seen on frontal X-ray in the upper paramediastinal lung due to angulation of the medial part of the fissure.
Boundaries and Pleural Recesses
The pleura extends 2 to 3 cm above the first rib, rising beneath the sternocleidomastoid muscle to cover the cupola or dome of the lung. Inferiorly, the pleura follows the line of attachment between the diaphragm and chest wall, ending at the level of the 6th or 7th rib anteriorly, coursing obliquely laterally, and reaching below the 12th rib posteriorly 1 , 6 (Fig. 5‑10). Although predominantly protected by the bony thorax, the pleura is vulnerable to injury above the medial first rib, below the costo-xiphisternal angle anteromedially on the right, and posteromedially below the bilateral costovertebral angles. 4
The pleural recesses are potential spaces located in regions where the parietal pleura changes direction (Fig. 5‑10 , Fig. 5‑11 , Fig. 5‑12). They are present bilaterally at expiration and fill in with lung during inspiration and include the anterior and posterior costomediastinal recess, costophrenic recess, and mediastinophrenic recess 1 , 4 (Fig. 5‑11). The anterior costomediastinal recesses are located between the anterior costal pleura and mediastinal pleura and extend from the sternoclavicular joints down to the seventh costal cartilages (Fig. 5‑12). The interpleural triangles denote the spaces separating the right and left anterior costomediastinal recesses superiorly and inferiorly (Fig. 5‑12). The left anterior costomediastinal recess may be larger than the right due to the cardiac notch in the left lung. The posterior costomediastinal recesses are located between the mediastinal and posterior costal pleura and extend from the first rib to the 11th intercostal space. Extension of the mediastinal pleura between the hilum or inferior vena cava anteriorly and the vertebral body posteriorly is known as azygoesophageal recess because it is delimited by the esophagus/azygos vein medially (Fig. 5‑12). Medial margin of this recess can be seen on frontal chest X-rays as a linear line anterior to the spine (Fig. 5‑11). The costophrenic recesses (lateral and posterior) are located at the junction between the costal and diaphragmatic pleura and extend from the 7th costal cartilage anteriorly to the neck of the 12th rib posteriorly (Fig. 5‑12). The mediastinophrenic recesses are located between the mediastinal and diaphragmatic pleura and extend from the posterior aspect of the sternum to the posterior 11th intercostal space. The right mediastinophrenic recess is associated with the pericardium, right phrenic nerve, right atrium, inferior vena cava, right border of the esophagus, and right vagus nerve. The left mediastinophrenic recess is associated with the pericardium, left phrenic nerve, left ventricle, esophagus, left vagus nerve, and descending thoracic aorta. 7









Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree