Diagnosis: Aneurysmal subarachnoid hemorrhage
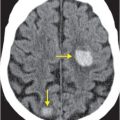
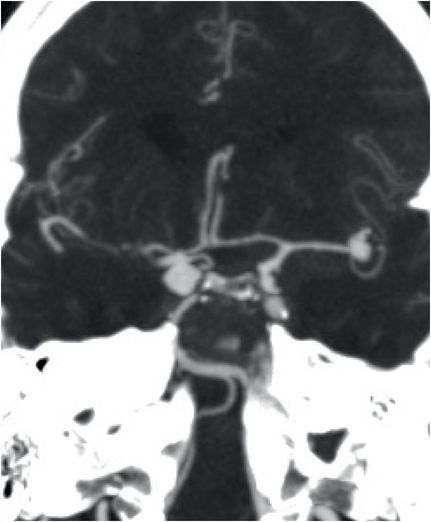
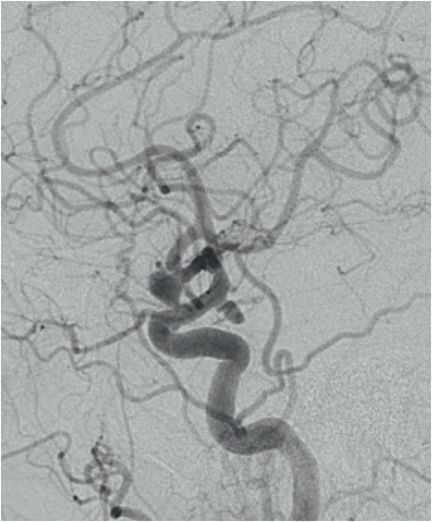
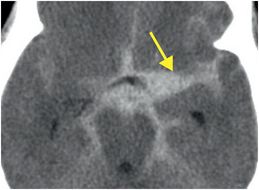
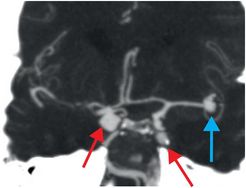
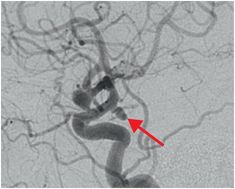
Noncontrast head CT (left image) shows diffuse subarachnoid hemorrhage, more prominent on the left (yellow arrow). Coronal CTA MIP reconstruction (middle image) and lateral view of a cerebral angiogram of left internal carotid artery injection (right image) show multiple aneurysms of both posterior communicating arteries (Pcom; red arrows) and the left MCA bifurcation (blue arrow).
Discussion
Diffuse subarachnoid hemorrhage (SAH) secondary to aneurysm rupture classically presents as rapid onset of the worst headache of a patient’s life. Associated symptoms may include retro-orbital pain, double vision, seizures, cognitive impairment, and vomiting.
The Hunt and Hess scale is a clinical scoring system that was developed in 1968 to classify the severity of a subarachnoid hemorrhage in order to predict patient prognosis.
| Grade | Description | Survival |
|---|---|---|
| 0 | No deficit or discomfort | |
| I | Headache but no neurological impairment | 70% |
| II | Cognitive impairment or difficulty in arousal | 60% |
| III | Cognitive/arousal deficit and limb deficit (power, tone, and/or sensation) | 50% |
| IV | Unconscious with marked changes in limb tone, power | 20% |
| V | Unresponsive | 10% |
| **** | Add one grade if major concurrent heart, lung, liver, renal pathology. |
Risk factors for aneurysm rupture
The usual cause of aneurysmal subarachnoid hemorrhage is rupture of a “berry” or saccular aneurysm at the circle of Willis or its branches that has formed as a result of weakness of the vessel wall. Most commonly, aneurysms form at the anterior communicating artery (ACom, ~30%), posterior communicating artery (PCom, ~30%), MCA bifurcation (MCA, ~30%), and posterior circulation (~10%, with the basilar tip constituting ~90% of this group).
Aneurysms more than 1 cm in diameter are more likely to bleed than those <5 mm. Larger aneurysms are much less common than smaller aneurysms. Although larger aneurysms are more prone to rupture, smaller aneurysms are implicated in the majority of cases of SAH. Intracranial aneurysms are multiple in about one-third of patients.
Intracranial aneurysms tend to affect patients from 35 to 60 years of age with a female-to-male ratio of 3:2. Other risk factors for aneurysmal SAH include black race, hypertension, autosomal dominant polycystic kidney disease, smoking, heavy alcohol use, first-degree relative with SAH, and disorders of abnormal connective tissue.
Fusiform aneurysms may arise from atherosclerotic or traumatic etiologies, while smaller, peripherally located mycotic aneurysms are seen in patients with endocarditis or other infectious causes.
Intracranial aneurysms affect approximately 1–5% of the population. Overall, 0.2–3% of the population suffers from intracranial aneurysm rupture each year. 10 to 15% of patients die before reaching the hospital, and 40–50% of patients die within 30 days.
The risk of recurrent aneurysmal hemorrhage on the first day is 4%, with an additional 1.2% risk each subsequent day for the first 2 weeks. Subarachnoid hemorrhage places the patient at risk for communicating hydrocephalus by causing blockage of the arachnoid granulations, which perform fluid exchange between the CSF and venous sinuses. Evaluation and monitoring of ventricular size is essential early on.
Vasospasm
Delayed cerebral ischemia as a result of vasospasm is a common complication of SAH that may double the mortality rate. Vasospasm occurs in approximately 50–70% of patients with SAH and delayed cerebral ischemia occurs in approximately 19–46%. Vasospasm is thought to account for up to 23% of disability and death related to SAH.
Vasospasm tends to occur between days 5 and 10 after SAH with the onset of new neurological symptoms. Transcranial Doppler and cerebral angiography are sometimes used to complement clinical surveillance for this complication. Calcium channel blockers (nimodipine, verapamil) and “HHT” (hypervolemic hypertensive therapy) are established treatments for vasospasm.
The Fisher CT grading scale, which identified vasospasm as a major cause of morbidity due to delayed ischemia in patients with SAH, was developed in 1980. This scale, among others, is used to estimate the risk for vasospasm based on the amount of subarachnoid hemorrhage.
| Grade | Amount of subarachnoid hemorrhage |
|---|---|
| 1 | None evident |
| 2 | Less than 1 mm thick |
| 3 | More than 1 mm thick |
| 4 | Any thickness with intraventricular or parenchymal hemorrhage |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree