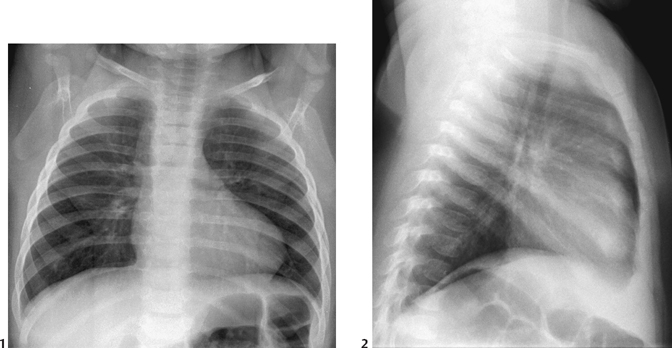
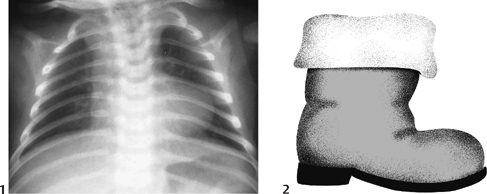
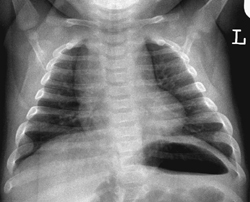
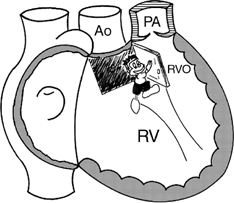
CASE 50 A 2-month-old infant presents with cyanosis. Figure 50A A frontal chest radiograph (Fig. 50A1) shows situs solitus and levocardia. The heart is normal in size, but its apex is uplifted, and the pulmonary arterial segment is flat. The overall cardiac configuration is boot shaped. The aortic arch is right sided. The pulmonary vascularity is decreased, which is more evident in the lateral view (Fig. 50A2). The perception in the lateral view can be facilitated by one’s level of familiarity with normal vascularity. Figure 50B Frontal chest radiograph (1) of a patient with pulmonary atresia with ventricular septal defect and small patent ductus arteriosus. The cardiac configuration is very similar to a boot (2). Figure 50C Frontal chest radiograph obtained in a lordotic projection from a normal infant shows a cardiac configuration similar to those of Figs. 50A1 and 50B1. Tetralogy of Fallot with a right aortic arch. A chest frontal view of another patient with tetralogy and pulmonary atresia shows more typical appearance of a boot (Fig. 50B). Boot-shaped heart: The severity of the pulmonary outflow tract obstruction is the key as to when children with tetralogy begin to manifest significant symptoms and signs. Infants with a moderate degree of pulmonary outflow tract obstruction do well for the first few months of life with minimal or no evidence of cyanosis. With milder degree of obstruction, the patients can develop congestive heart failure due to left-to-right shunt. These patients develop cyanosis or cyanotic spells later in life as the pulmonary outflow tract becomes narrower, allowing right-to-left shunt. Severe cyanosis and hypoxemia in the newborn period means that the obstruction is severe or there is pulmonary atresia. Figure 50D Cartoon showing pathogenetic mechanism of tetralogy of Fallot. The trap door is the outlet or infundibular septum. Ao, aorta; PA, pulmonary artery; RV, right ventricle; RVO, right ventricular outflow. The four components of tetralogy of Fallot are a ventricular septal defect, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy. The first three components are in fact the consequences of a single pathogenetic mechanism: the anterior, superior, and leftward deviation of the outlet septum in relation to the rest of the ventricular septum (Fig. 50D
Clinical Presentation
Radiologic Findings
Diagnosis
Differential Diagnosis
Discussion
Clinical Findings
Pathology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree