

Diagnosis: Cocaine-induced vasoconstriction syndrome
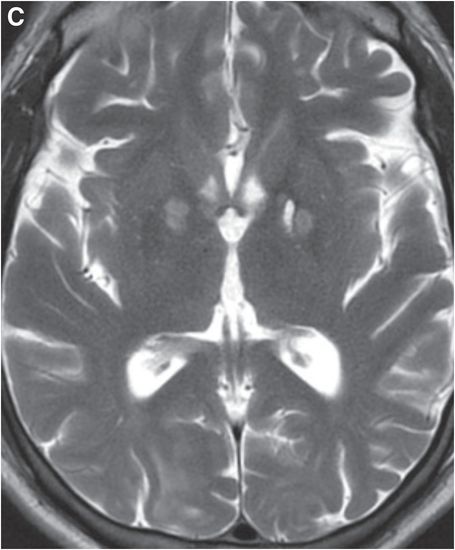
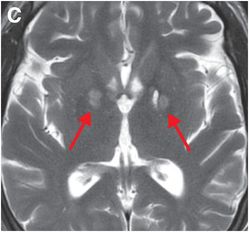
Axial T2 (A) and DWI (B) MR images demonstrate T2 prolongation and reduced diffusion, consistent with acute bilateral cerebellar gray matter infarcts (yellow arrows). Axial T2-weighted image at the level of basal ganglia (C) reveals T2 prolongation in the globus pallidi bilaterally (red arrows). DWI at that level (not shown) did not demonstrate reduced diffusion, indicating chronic infarction. Axial DWI at the level of the cerebral convexities (D) shows reduced diffusion consistent with acute bilateral cortical and subcortical infarction (blue arrows). The presence of multiple acute supratentorial and infratentorial infarcts is highly suggestive of vasoconstriction syndrome, of which cocaine is a known cause.

Discussion
Overview of street drug-induced neurological injury
Cocaine use can result in significant neurological injury due to neurovascular complications, such as hemorrhage, stroke, and arteriopathy.
Hemorrhage often results from transient blood pressure elevation due to the sympathomimetic action of the drug, and can occur in the brain parenchyma or subarachnoid space. Subarachnoid hemorrhage may be due to rupture of a pre-existing aneurysm or vascular malformation, or may result from extension of a parenchymal hemorrhagic infarct.
Ischemic stroke may result from vasoconstriction or “moyamoya-like” arteriopathy. Cocaine may further predispose to ischemic stroke by causing hypercoagulability.
Heroin inhalation injury, known as “chasing the dragon,” produces cerebellar white matter injury without cortical infarction.
Imaging of reversible cerebral vasoconstriction syndrome
Reversible cerebral vasoconstriction syndrome (RCVS) is characterized by hyperacute severe headache and multifocal vasospasm. The condition usually resolves by 3 months, but in severe cases may lead to permanent sequelae due to multiple infarcts. Together, vasoactive drugs and postpartum state account for more than half of cases. The distribution of abnormalities in RCVS is similar to that seen in posterior reversible encephalopathy syndrome (PRES), a syndrome thought to be due to loss of autoregulation of posterior circulation blood pressure. PRES is seen in diverse clinical scenarios, but most commonly in hypertension. On MRI, PRES typically features relatively symmetric hyperintensities on T2-weighted images, involving the cerebral convexities, cerebellum, and other territories. Acute infarcts, while still rare, are more common in RCVS.
In RCVS, MRA and CTA show multiple vascular narrowings, more severe than in PRES.
Treatment of RCVS
Anti-hypertensive agents, the mainstay of treatment in PRES, can worsen outcome in RCVS. RCVS is often treated with calcium channel blockers and steroids.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








