Diagnosis: Spondylodiscitis and paraspinal abscess
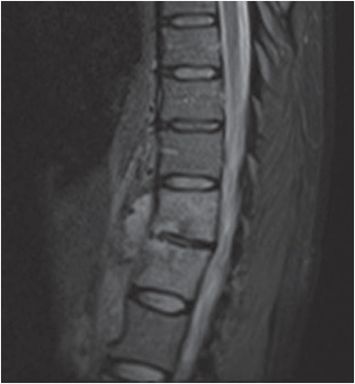
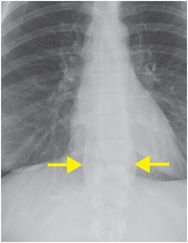
PA chest radiograph (left image) demonstrates lateral displacement of the right and left paraspinal lines (yellow arrows). Sagittal T1-weighted (middle image) and STIR (right image) MR images show low T1 and high T2 signal intensity of two consecutive vertebral bodies (red arrows), with loss of definition of the vertebral endplates. In addition, there is a prevertebral fluid collection (blue arrows) consistent with an abscess.


Discussion
Overview of spondylodiscitis
Spondylodiscitis is septic inflammation of the spine involving the intervertebral disc and adjacent vertebral bodies, often with extension into the paravertebral soft tissues. The lumbar spine is the most common site.
Spondylodiscitis has a bimodal age distribution, being more common in young (<20 years of age) and older (50–70 years of age) patients. Risk factors include diabetes, malignancy, compromised immunity, and intravenous drug use.
The spinal column may become involved by infection via several routes of spread. Vascular spread of infection is thought to be due to Batson’s paraspinal venous plexus. Contiguous spread of an adjacent infection can be seen in the setting of an infected aortic graft, mediastinal abscess, or retropharyngeal abscess. Direct contamination can be due to penetrating trauma or surgery.
Clinical symptoms are nonspecific, which can delay the diagnosis. Back pain in the setting of fever is considered a “red flag” that should prompt imaging, especially in the presence of leukocytosis or elevated inflammatory markers (elevated C-reactive protein or erythrocyte sedimentation rate).
Treatment is usually with antibiotics; however, if there is evidence of neurological compromise due to mass effect or large abscess, then surgery may be necessary.
Imaging of spondylodiscitis
Chest radiograph has low sensitivity and specificity, but may show thickening of the paravertebral soft tissues, as in the index case. Later findings include decreased intervertebral disc space and endplate irregularity, although degenerative disc disease may appear identical.
MRI is the preferred imaging modality when spondylodiscitis is suspected, due to its ability to identify paravertebral and epidural involvement, as well as involvement of the spinal cord itself. Findings consist of loss of definition of the affected vertebral endplates, with low signal intensity on T1-weighted images, and corresponding high signal intensity on T2/STIR images. Fluid-like signal may also be seen in the disc space and can help to differentiate infectious discitis from degenerative disc changes. In degenerative disease, the disc is typically dehydrated, demonstrating low T2 signal intensity (although this is variable). Post-contrast images may demonstrate a phlegmon or an abscess in the paravertebral soft tissues, the former demonstrating heterogeneous enhancement, and the latter, peripheral enhancement. In treated cases, follow-up MRI may show resolution of edema with fatty or sclerotic charges.
Computed tomography can also be performed in the acute setting due to its ready availability. CT may demonstrate decreased intervertebral disc space and vertebral endplate irregularity and destruction, and can assess paravertebral soft tissue involvement, such as presence of phlegmon or abscess. CT is also a useful modality for pretreatment planning, such as percutaneous drainage of abscess or biopsy of the intervertebral disc. While degenerative disc disease may appear similar to spondylodiscitis on CT, it is important to note that the presence of gas in the intervertebral disc is considered pathognomonic for degenerative disc disease.
Clinical synopsis
The patient had a history of IV drug use. She was admitted, and after becoming afebrile, she was discharged with 6 weeks of IV antibiotic therapy (nafcillin). Post-treatment imaging of the spine demonstrated resolution of the paravertebral abscess.
Self-assessment
Spectrum of spondylodiscitis
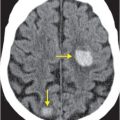
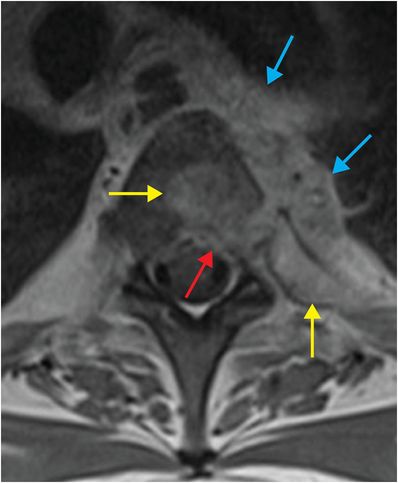
Bacterial spondylodiscitis complicated by epidural phlegmon
Infection of the spine may involve the adjacent soft tissues, including the paraspinal region (as in the index case) or the epidural space. Epidural spread may be a cause of spinal cord compression. Axial T1-weighted post-contrast MR of the thoracic spine demonstrates enhancement of the posterior aspect of the vertebral body and medial left rib (yellow arrows). There is posterior cortical breakthrough into the anterior spinal canal with lobulated, heterogeneously enhancing phlegmon extending to the epidural space (red arrow). An extensive left-sided prevertebral abscess (blue arrows) causes esophageal displacement to the right.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree