Diagnosis: Diffuse axonal injury
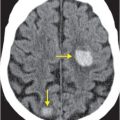
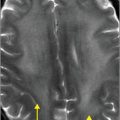
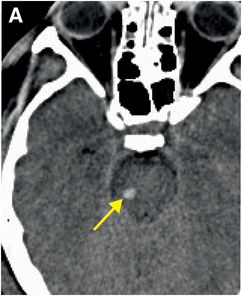
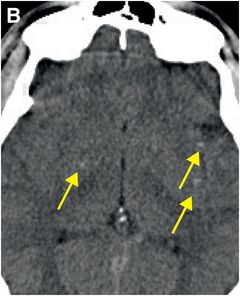
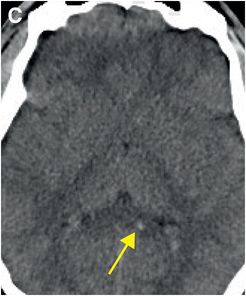
Unenhanced axial CT images (A–C) show multiple small foci of hemorrhage (arrows) in the right pons (A), right basal ganglia, left subinsular region (B) and left splenium of the corpus callosum (C).
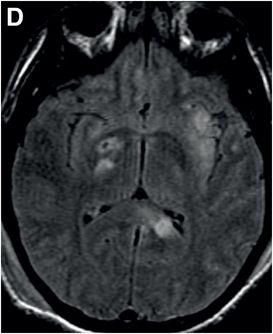
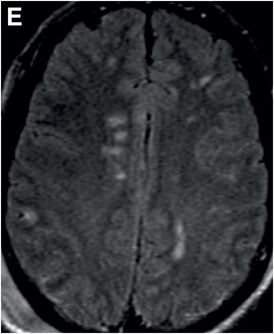
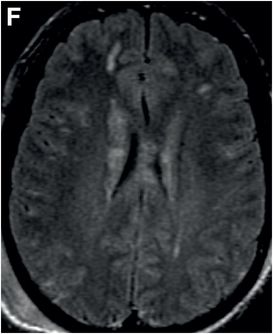
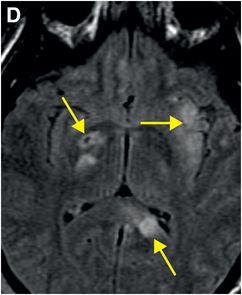
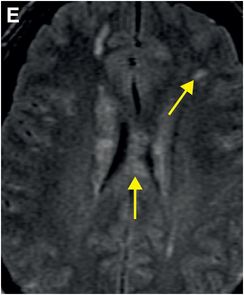
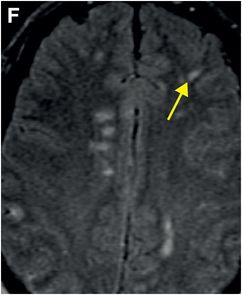
Axial FLAIR MR images (D–F) demonstrate multiple corresponding signal abnormalities in the basal ganglia, subinsular region, splenium (D) and body of the corpus callosum (E) as well as gray–white junctions (E, F).
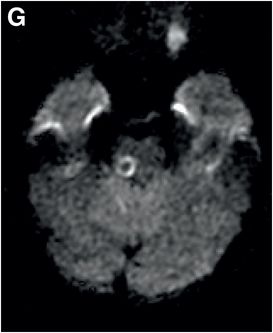
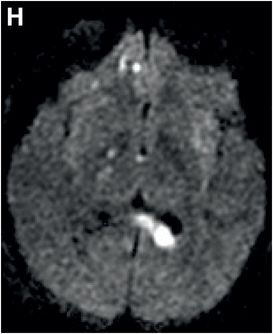
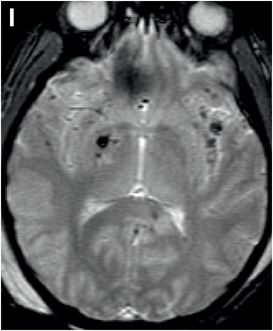
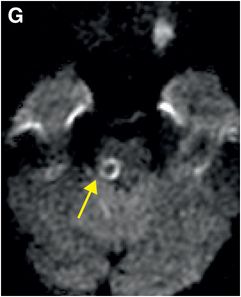
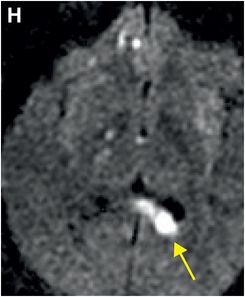
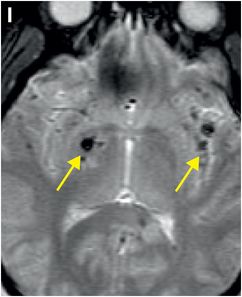
Axial diffusion-weighted imaging (DWI) (G, H) and gradient-recalled echo (GRE) (I) images show corresponding bright DWI and dark GRE foci in the right pons (G), left splenium (H), right basal ganglia, and left subinsular regions (I).
Discussion
Overview of diffuse axonal injury
Diffuse axonal injury (DAI) is a common, potentially devastating traumatic brain injury resulting from acceleration–deceleration or rotational forces, such as those that occur in high-speed motor vehicle accidents, assaults (including child abuse), and falls.
DAI is implicated in the majority of cases of unconsciousness and vegetative state after closed head injury. Most patients (90%) with severe DAI remain in a coma. Those who regain consciousness are often left with significant residual neurological deficits. Some experts consider concussion to be a mild manifestation of DAI.
Pathophysiology of DAI
Microscopically, DAI reflects axonal disruption due to shear forces that stretch the axons as different density tissues slide across each other during injury. Axons that bridge the gray–white (corticomedullary) junction are therefore most commonly involved.
Generally, it is not mechanical force itself that disrupts axons, but rather a precipitation of biological cascades that occurs over hours to days after the time of impact.
Cytoskeletal and axonal cell membrane (axolemma) injury are key pathophysiological features. Stretching damages the cytoskeleton with disruption of sodium and calcium channels, leading to mitochondrial dysfunction and eventual cell death. Axonal transport is compromised at the site of cytoskeleton injury, resulting in accumulation of transported materials. The axon swells and ultimately tears, retracting toward the cell body and forming the so-called “retraction ball” that is a characteristic histological feature of DAI.
Downstream from the initial injury, Wallerian degeneration begins within 1–2 days.
Imaging of DAI
On imaging, DAI manifests as small lesions (1–15 mm) in the white matter, commonly at the corticomedullary junction, corona radiata, corpus callosum, brainstem, basal ganglia, and thalami.
Initial CT is often normal (50–80%), with limited sensitivity due to the small size and the temporal evolution of DAI lesions. One should, therefore, always consider DAI when neurological deficits are disproportionate to imaging findings after typical injury mechanisms such as high-speed motor vehicle accident (MVA).
Compared to CT, diffusion-weighted MRI is much more sensitive for detecting punctate foci of cytotoxic edema, and GRE MRI is more sensitive for micro-hemorrhage (susceptibility effects).
Ongoing research efforts focus on using magnetization transfer, diffusion tensor imaging (DTI), and perfusion imaging to gauge the degree of injury and, perhaps, to predict outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree