
Diagnosis: Grade 3 splenic laceration with splenic artery pseudoaneurysms
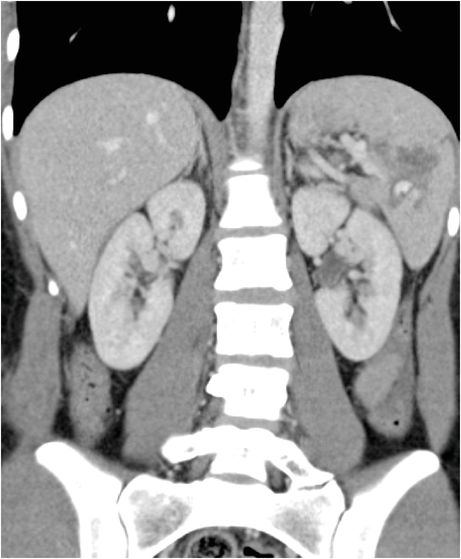
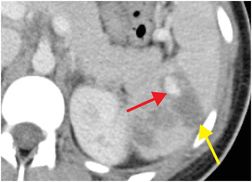
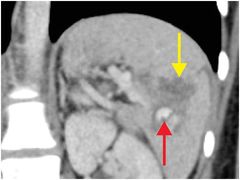
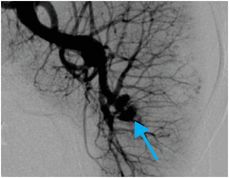
Axial (left image) and coronal (middle image) enhanced CT demonstrate an irregular, low-attenuation defect (yellow arrows) in the spleen greater than 3 cm in length, consistent with a grade 3 laceration. There is a round focus of increased attenuation adjacent to the laceration (red arrows) that is similar in attenuation to the arterial tree, consistent with a vascular injury (active extravasation or pseudoaneurysm). Subsequent digital subtraction angiogram (right image) of the splenic artery confirms the presence of two adjacent pseudoaneurysms in the lower pole of the spleen (blue arrow).
Discussion
Overview of splenic trauma
The spleen is the abdominal organ that is most often injured in trauma. The majority of splenic injuries are caused by blunt abdominal trauma. Associated injuries frequently involve the left hemithorax, pancreatic tail, and left hepatic lobe.
Imaging of splenic trauma
Contrast-enhanced CT is the imaging modality of choice in suspected splenic trauma. Splenic laceration appears as a low-attenuation, irregular, linear, or wedge-shaped hypodense defect extending from the splenic margin. It may be associated with hemoperitoneum, active extravasation, pseudoaneurysm, or subcapsular hematoma.
High-grade injuries may result in vascular disruption, which can be seen as active extravasation or a traumatic pseudoaneurysm, as in the index case. Contrast extravasation or “blush” on CT suggests active hemorrhage.
Grading of splenic trauma
Treatment of splenic trauma
Treatment of traumatic splenic injury varies by institution.
Imaging findings are critical to the multidisciplinary management of the patient, as the natural course may vary from spontaneous hemostasis to hemodynamic instability. While the former is often managed with watchful waiting or serial imaging, the latter requires emergent transcatheter embolization or splenectomy.
Due to the deleterious effects of splenectomy on immune function, the trend is for conservative treatment except in unstable or potentially unstable patients.
Clinical synopsis
The patient underwent successful angiographic coil embolization of the splenic artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








