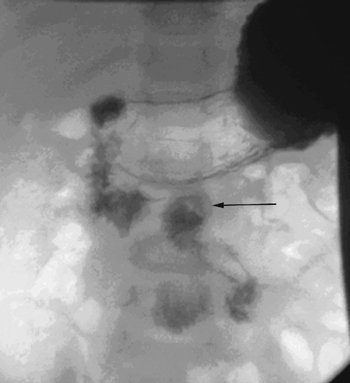
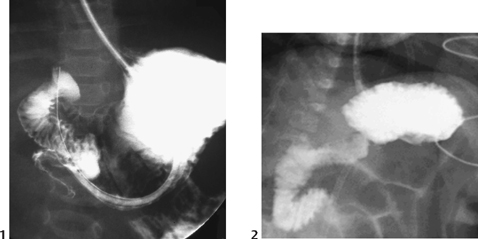
CASE 62 A 3-week-old boy presents with sudden-onset bilious vomiting. Figure 62A Upper gastrointestinal (GI) study (Fig. 62A) demonstrates an abnormally low position of the duodenojejunal junction (DJJ) (arrow), below the level of the duodenal bulb. Figure 62B Abdominal x-ray of a 5-month-old girl presenting in hypovolemic shock. Thickened bowel loops secondary to ischemia are seen in the left upper quadrant. Malrotation Malrotation and midgut volvulus is potentially one of the most serious pediatric surgical emergencies, and the role of radiology in its diagnosis is critical. Delay in diagnosis carries the risk of infarctive necrosis of the entire small bowel and is potentially fatal. Figure 62C Signs of volvulus on upper GI study include the classic “corkscrew” appearance (1) and almost complete obstruction of the third part of the duodenum (2). Eighty to 90% of children present with bilious vomiting at <1 year of age, 65 to 75% within the first month of life. However, volvulus can occur at any age, including adulthood, and the diagnosis should always be considered. Late presentation can result in a hypovolemic, shocked patient. In older children, intermittent obstruction can cause chronic or recurrent abdominal pain, vomiting, and failure to thrive. Rarely, a malabsorption syndrome results from chronic venous and lymphatic obstruction. Melena due to bleeding from mesenteric and intramural varices secondary to chronic venous obstruction has been described.
Clinical Presentation
Radiologic Findings

Diagnosis
Differential Diagnosis
Discussion
Background
Etiology/Embryology
Clinical Findings
Associated Conditions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree