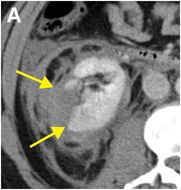
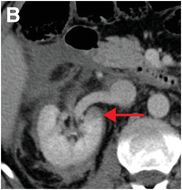
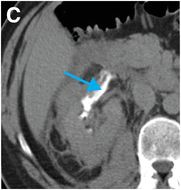
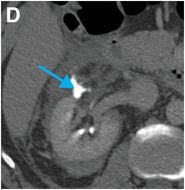
Diagnosis: Renal laceration extending into the collecting system (Grade IV traumatic renal injury)
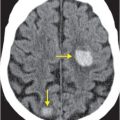
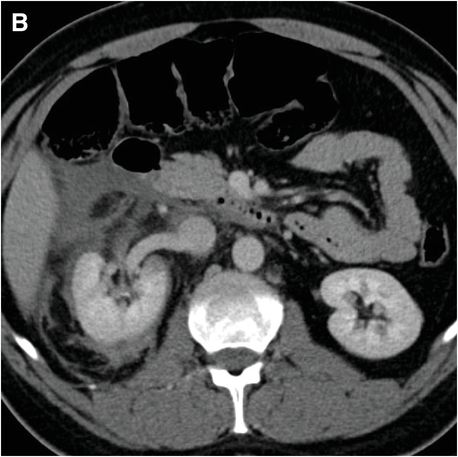
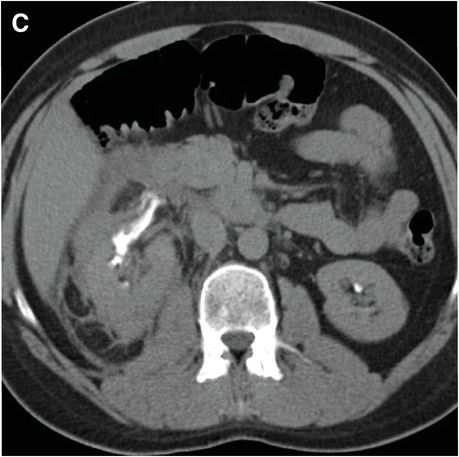
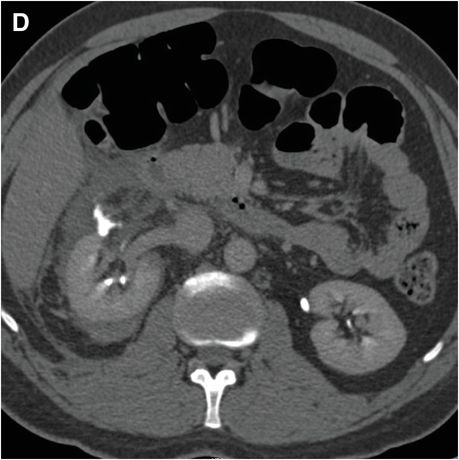
Contrast-enhanced axial CT (A,B) demonstrates a deep right renal laceration (yellow arrows) with hyperdense, hemorrhagic perinephric fluid. A small hypoenhancing parenchymal contusion is also seen medially (red arrow). Delayed, excretory phase axial images (C,D) show excreted contrast leakage from the injured collecting system (blue arrows).
Discussion
Overview of renal trauma
The kidneys are the most commonly traumatically injured organ in children and the third most commonly injured organ (after the spleen and liver) in adults. Blunt trauma accounts for 90% of renal injuries.
Imaging of suspected renal injury
Imaging is not essential in every case of suspected renal injury. Established indications for imaging differ for adults and pediatric patients, and also depend on the mechanism of injury (blunt versus penetrating injury).
Blunt abdominal trauma in adults: patients with gross hematuria OR microscopic hematuria with shock (systolic blood pressure <90 mmHg) should be imaged. Microscopic hematuria in the absence of shock is not an indication for imaging.
Blunt abdominal trauma in children: patients with microscopic or gross hematuria should be imaged, irrespective of blood pressure.
Penetrating trauma: all patients, irrespective of age or whether hematuria is present, should be imaged.
Contrast-enhanced CT is the primary modality for assessing renal injury. Imaging during multiple phases of enhancement is often required for adequate evaluation of the renal parenchyma, vasculature, and collecting system. Routine images are obtained in the portal venous phase. Delayed phase images, if necessary, are typically obtained 3–5 minutes after the initial injection of contrast material. Ideally, a radiologist is present at the CT scanner at the time of imaging to decide whether delayed phase images are needed.
If a renal laceration is detected during the portal venous phase, or if there is unexplained perinephric fluid, a delayed scan should generally be performed to assess for extension of injury into the collecting system. Extravasation of opacified urine from the collecting system confirms this injury.
If a contrast blush is detected on the portal venous phase, delayed imaging (in a hemodynamically stable patient) can help differentiate a contained traumatic pseudoaneurysm or arteriovenous fistula from active intraparenchymal bleeding: free contrast extravasation persists on delayed phase imaging, while the contained vascular injuries will wash out. Stable patients with active bleeding (persistent and/or enlarging contrast blush) are often referred for emergent angiographic embolization.
Classification of traumatic renal injuries
Various classification systems exist. The most commonly referenced grading system is the organ injury scale (OIS) from the AAST.
| Grade | Injury description | |
|---|---|---|
| I | Contusion | Microscopic or gross hematuria |
| Hematoma | Subcapsular, nonexpanding hematoma without laceration | |
| II | Hematoma | Nonexpanding perirenal hematoma confined to renal retroperitoneum |
| Laceration | <1 cm parenchymal depth of renal cortex without urinary extravasation | |
| III | Laceration | >1 cm parenchymal depth of renal cortex without urinary extravasation or collecting system rupture |
| IV | Laceration | Parenchymal laceration extending through the renal cortex, medulla, and collecting system |
| Vascular | Traumatic thrombosis of a segmental renal artery branch or injury to the main renal artery without complete renal devascularization | |
| V | Laceration | Completely shattered kidney |
| Vascular | Avulsion of the renal hilum with complete renal devascularization, or traumatic main renal artery thrombosis | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree