CASE 64
Clinical Presentation
A 6-year-old boy presents to the emergency department with a 24-hour history of lower abdominal pain and fever.
Figure 64A
Radiologic Findings
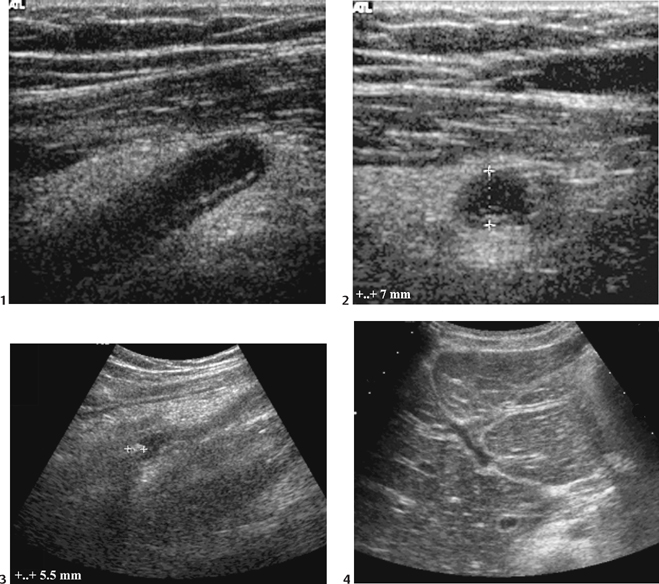
Longitudinal (Fig. 64A1) and transverse (Fig. 64A2) ultrasound images demonstrating a fluid-filled tubular structure in the right iliac fossa (7 mm diameter), which was noncompressible and could be traced to the cecum. A 5.5 mm high echogenicity focus with acoustic shadowing is seen at the base (Fig. 64A3); the surrounding mesenteric fat is markedly echogenic, and increased periportal echoes are noted in the liver (Fig. 64A4).
Diagnosis
Acute appendicitis with appendicolith
Differential Diagnosis
- Normal appendix: blind-ending and in continuity with the cecum, but ≤6 mm in diameter and without hyperemia or surrounding inflammatory changes
- Normal terminal ileum: not in continuity with the cecum, not blind-ended, and shows frequent peristalsis
- Terminal ileitis: thickened, hypoperistaltic terminal ileum of inflammatory or infectious etiology
- Mesenteric adenitis: multiple small mesenteric lymph nodes and small amounts of free fluid, but the appendix appears normal
- Colitis (e.g., Crohn’s disease, typhlitis, pseudomembranous colitis): may involve the appendix, but more extensive colonic thickening and pericolic inflammatory changes should allow differentiation
Discussion
Background
Acute appendicitis is the most common acute surgical condition in childhood, with a lifetime risk of 7 to 9%. The optimal imaging and diagnostic strategy is one of the most currently controversial topics in pediatric radiology.
Etiology
- The presence of an appendicolith (inspissated fecal material and inorganic salts) in ~50% of cases suggests that luminal obstruction is a central etiologic factor. Luminal distension, ischemia, and secondary bacterial infection follow. Inflammatory changes spread from the mucosa through the appendiceal wall to the serosa. Necrosis of the appendiceal wall results in perforation, abscess formation, and peritonitis.
- In a small number of cases, appendiceal obstruction is secondary to foreign bodies, parasites, or neoplasms (e.g., carcinoid, adenocarcinoma, lymphoma).
Clinical Findings
Peak age of presentation is between 10 and 15 years of age. However, appendicitis may occur at any age, including in children as young as 1 year of age. Classic presentation is with ill-defined abdominal pain moving to the right iliac fossa, accompanied by fever, vomiting, and a raised white cell count. However, the diagnosis is often more complex in adolescent girls, in whom gynecologic conditions may show similar presentation. In young children, an atypical presentation with malaise, anorexia, vomiting, and diarrhea is more common. Delay in diagnosis is relatively common in children <10 years of age, especially in infants/toddlers, many of whom present following a 1- to 2-week history of pain with established pelvic abscesses secondary to perforation.
Complications
Pathology
- Macroscopically, the appendix is congested, the lumen commonly distended with pus and containing an obstructing fecolith. The serosa may be covered with exudate.
- Microscopically, mucosal ulceration and neutrophilic infiltration are required for diagnosis. Transmural inflammation with necrosis and perforation and/or serosal inflammation with periappendicitis are also frequently present.
Imaging Findings
ABDOMINAL RADIOGRAPHY
- Of low sensitivity and specificity and therefore not recommended as routine
- Often normal or shows nonspecific findings of right iliac fossa inflammation such as localized dilated loops, an indistinct right psoas margin, loss of the right-sided properitoneal or obturator internus fat planes, and scoliosis convex to the left
- A radiodense appendicolith is highly specific in the symptomatic patient but only seen in 5 to 10% cases.
- Generalized small bowel dilatation may indicate partial obstruction from a localized phlegmon/ abscess or paralytic ileus secondary to generalized peritonitis.
- Free air is very uncommon.
ULTRASOUND