Diagnosis: Uterine perforation as a complication of therapeutic abortion
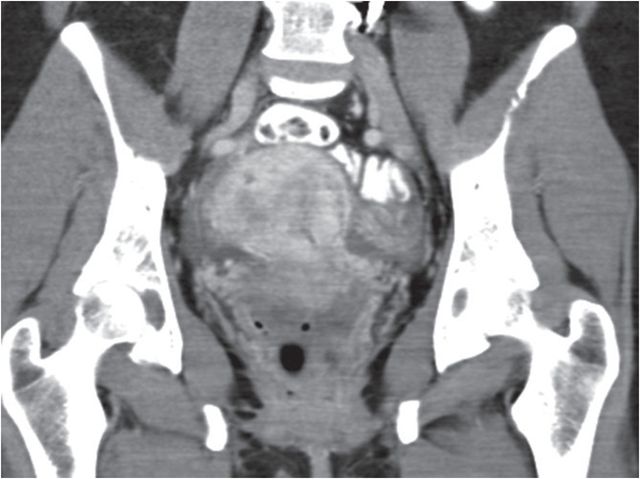
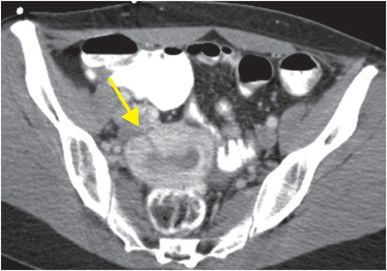
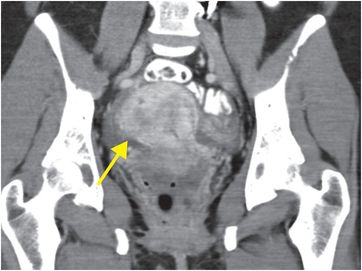
Axial and coronal contrast-enhanced CT of the pelvis show a linear low-attenuation defect (arrows) through the right anterior, inferior wall of the uterus and a small amount of free fluid, consistent with focal uterine perforation secondary to instrumentation.
Discussion
The majority of patients with uterine rupture have a history of prior cesarean section.
Uterine rupture most commonly occurs in women of childbearing age during pregnancy, labor, or the postpartum period. Uterine perforation may also occur due to instrumentation or trauma. Any site of prior uterine incision is predisposed to perforation.
Classic vertical cesarean section scars are more likely to rupture before labor, while transverse lower uterine segment scars more frequently rupture during or after labor.
Overall, the most common site of rupture is the anterior lower uterine segment, which is the thinnest portion of the myometrium in pregnant patients and the most common site of scarring from prior low transverse cesarean section.
Less commonly, rupture of the uterine body occurs during pregnancy.
Ultrasound, MRI, or CT can be used to evaluate suspected uterine rupture.
All modalities may demonstrate an extrauterine hematoma, ascites, or hemoperitoneum.
Ultrasound may show discontinuity in the myometrium with protrusion of the amniotic sac in a pregnant patient.
MRI may be most useful when anatomy is difficult to delineate by ultrasound, for instance in the presence of multiple fibroids or congenital fetal anomalies. MRI findings include a linear defect with high signal on both T1- and T2-weighted images that is clearly distinct from the normal incision site. CT is readily available in the acute setting and may demonstrate analogous findings.
If the patient is pregnant with a viable fetus, radiation dose should be considered in the risk–benefit analysis.
Clinical synopsis
The patient was admitted to the hospital. Since the myometrial defect was small, the patient was treated with antibiotics.
Self-assessment
|
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








