Diagnosis: Obstructive right ureterovesical junction (UVJ) stone with a pelvic kidney
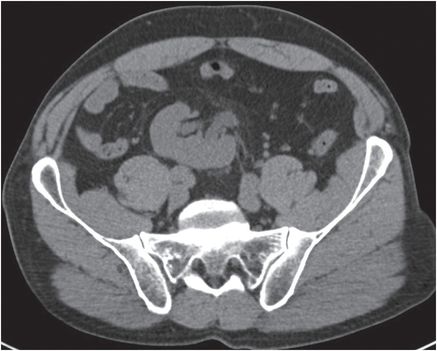
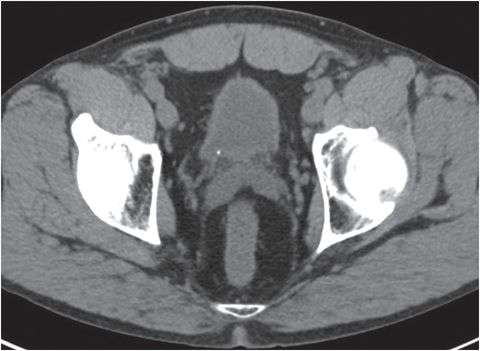
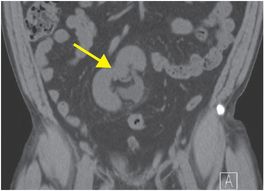
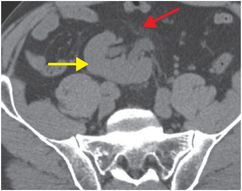
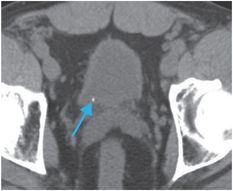
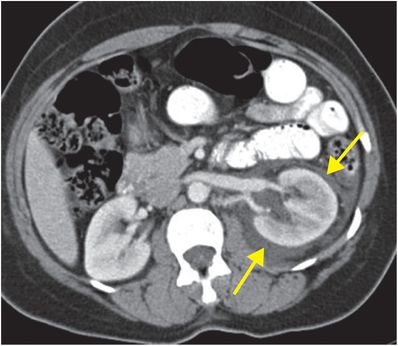
Coronal (left image) and axial (middle image) unenhanced CT images demonstrate a pelvic right kidney (yellow arrows) with mild hydroureteronephrosis. There is mild perinephric fat stranding, indicating an acute process (red arrow). Axial image through the bladder (right image) demonstrates a punctate, obstructing calcified stone at the right UVJ (blue arrow).
Discussion
Unenhanced CT is highly sensitive (97%) and specific (96%) for the detection of renal and ureteral stones.
Unenhanced CT is usually the preferred modality for the evaluation of renal and ureteral stone disease because of its ability to resolve between calcified stones, dense non-calcified concretions, and normal renal parenchyma. CT may also detect pathology in other organs that mimics renal colic.
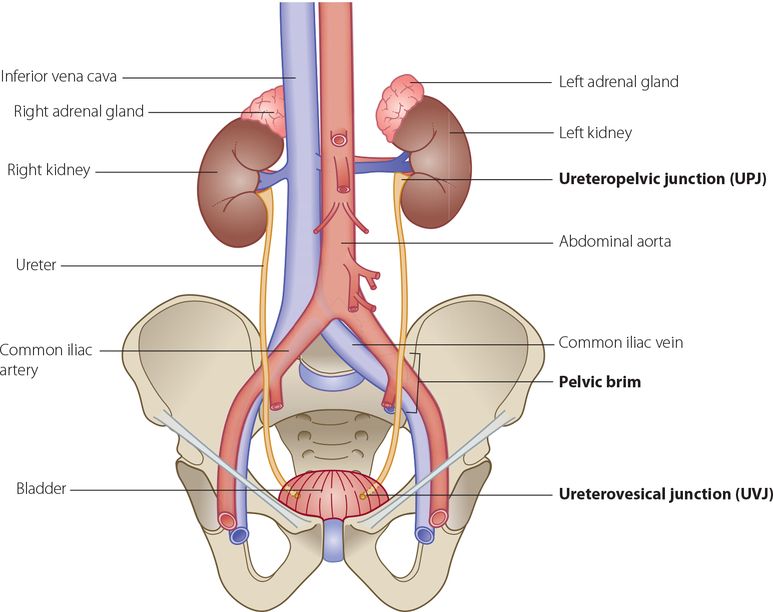
Initial ultrasound rather than CT may be selected for follow-up in patients with known stone disease or in young patients in whom diagnostic testing without ionizing radiation exposure is desired. However, focused ultrasound for nephroureterolithiasis can be technically challenging and is insensitive for small stones, stones at the ureteropelvic junction (UPJ), and stones in the mid ureter. Estimation of stone size may be inaccurate. Ultrasound is more useful in cases of stones >5 mm and cases with hydroureteronephrosis. In most cases with a negative ultrasound and ongoing concern for stone disease, unenhanced CT is performed. Stones are seen as echogenic foci with posterior acoustic shadowing. Absence of a “ureteral jet” in the bladder on the affected side may be seen with Doppler imaging.
The most common cause of calcification/calcium density in the renal parenchyma is nephrolithiasis. Medullary nephrocalcinosis and vascular calcification sometimes confound the diagnosis.
Dual-energy CT is an emerging technique that helps distinguish between uric acid and non-uric acid stones.
Dual energy CT acquires images with two x-ray tubes set 90 degrees apart that simultaneously scan the patient at higher (140 kVp) and lower (80 kVp) energy levels. Because different types of stones have different chemical composition, and hence k-edges, they absorb photons differently at different energy levels. The composition of different stones can be reliably predicted by calculating a ratio of the attenuation at low and high energy levels.
The distinction between uric acid and non-uric acid stones may be clinically important because some uric acid stones are treated with pharmacologic urine alkalinization rather than invasive procedures.
The most common locations of obstruction by ureteral calculi are in areas of normal ureteral narrowing.
Special attention should be paid to these areas when evaluating for stones:
A pelvic venous phlebolith may be differentiated from a ureteral calculus by the “soft tissue rim” sign, which represents the thickened, inflamed ureteral wall around the calcification. If this is present, it is more likely that the calcification represents a ureteral calculus.
Urosepsis may complicate obstructive uropathy from upper tract stones. Emergent procedures to decompress the collecting system are necessary.
Ureteral stents or percutaneous nephrostomy tubes temporize until the patient has clinically stabilized.
Yoshimura et al. published that the strongest risk factors for requiring emergent surgical drainage with obstructive calculi were poor performance status (e.g., spinal cord injury), female sex, and age >75.
Clinical synopsis
Because this patient’s stone was only 2 mm in diameter, the patient was managed conservatively with fluids and pain control. The stone passed spontaneously, and the patient was discharged from the Emergency Department.
Self-assessment
|
|
|
|
|
|
Spectrum of renal stone disease
Forniceal rupture
Forniceal (calyceal) rupture results from elevated pressure in the renal collecting system leading to urinary extravasation around the affected kidney. The most common cause is obstructive renal calculi, followed by obstructing malignancy. In this case, there was an obstructing stone in the pelvic ureter (not shown). Portal venous phase axial enhanced CT (upper image) demonstrates mild hydronephrosis, perirenal fat stranding, and low-density fluid (arrows). Post-contrast axial CT obtained ten minutes after administration of IV contrast (in the delayed or excretory phase) shows contrast in the renal collecting system and extravasation into the perirenal space (arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








