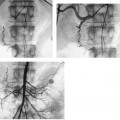
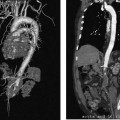
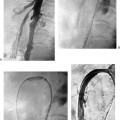
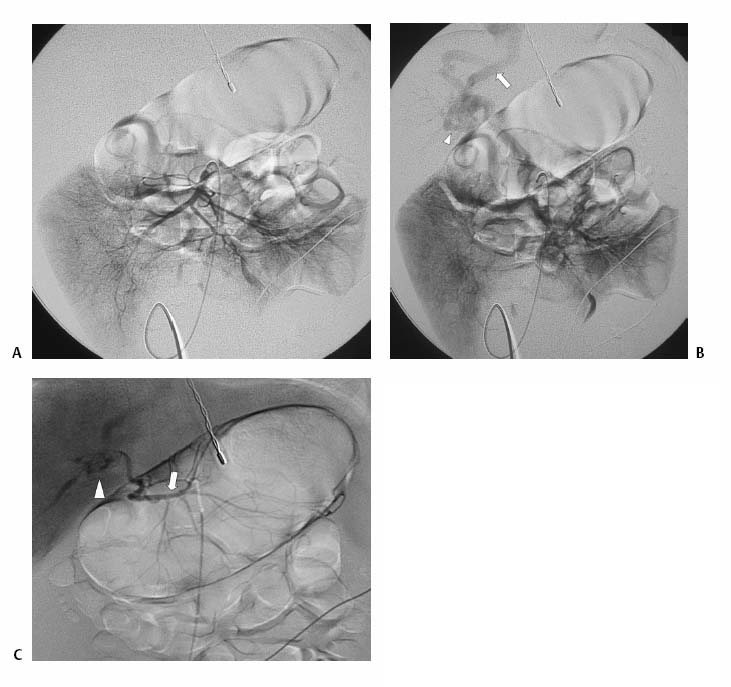
CASE 72 A newborn male presented with ascites and an elevated serum bilirubin level. Figure 72-1 (A) Newborn with abdominal distention and elevated liver function tests. Selected superior mesenteric arteriogram performed through the umbilical artery with a 3F visceral selective catheter shows normal arterial branching. (B) Venous phase shows evolving cavernous transformation of the portal vein (arrowhead) and patent intra-hepatic portal veins. Ductus venosus provides physiologic portosystemic shunt (arrow). (C) Late portal venous phase of a left gastric artery injection. Portal vein occlusion is only partial, as indicated by hepatopetal flow in the left gastric (coronary) vein (arrow) and thrombus in the distal main portal vein and proximal intrahepatic branches (arrowhead). Sonography with Doppler showed patent intrahepatic portal veins with sluggish flow. Selected mesenteric arteriography (Figs. 72-1A to C) performed through the umbilical artery showed a large filling defect within the distal portion of the main portal vein extending into the main intrahepatic branches. Portal vein thrombosis in a newborn. Under general anesthesia, the patient was placed supine on the angiography table, and the umbilical cord remnant and surrounding skin were prepped in sterile fashion. A 3-French (F) visceral selective catheter and a 0.018-inch Platinum Plus guidewire (Boston Scientific, Natick, Massachusetts) were used to access the umbilical artery. The superior mesenteric artery and the left gastric artery were selectively catheterized, and angiograms were performed through the portal venous phase of imaging. All angiograms were performed with hand injections of 3 to 5 cc of half-strength contrast material. Contrast material 3F visceral selective catheter (Cook, Bloomington, Indiana) 0.018″ Platinum Plus guidewire (Boston Scientific, Natick, Massachusetts) Portal venous thrombosis (PVT) is most common in young children but may occur in patients of any age from infancy to adulthood. Possible clinical presentations include abdominal pain, variceal bleeding, splenomegaly with associated hypersplenism, ascites, and neurocognitive deficits. PVT may be idiopathic or result from a wide variety of causes, including diffuse hepatic parenchymal diseases, inflammatory and infectious diseases of the abdominal cavity, dehydration, sepsis, hypercoagulable states, neoplastic diseases of the liver, and iatrogenic causes such as umbilical vein catheterization. In many cases, more than one risk factor is present. Symptoms of PVT tend to resolve or improve after restoration of outflow from the portal vein by a variety of radiologic and surgical treatments described below. Thus, early recognition of the clinical signs and symptoms and referral for diagnostic imaging are essential. Sonography with Doppler is the most common first-line imaging modality for PVT and may show absent or slow flow in the portal vein, intraluminal thrombus, and cavernous transformation, indicated by the presence of multiple, serpiginous periportal collateral veins in the porta hepatis. Extension of thrombus or development of collateral circulation may result in absent or hepatofugal flow in the splenic and superior mesenteric veins.
Clinical Presentation
Radiologic Studies
Diagnosis
Treatment
Equipment
Discussion
Background
Noninvasive Imaging Work-up
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree