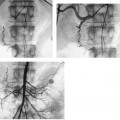
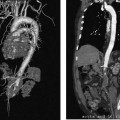
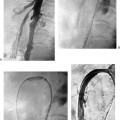
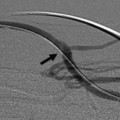
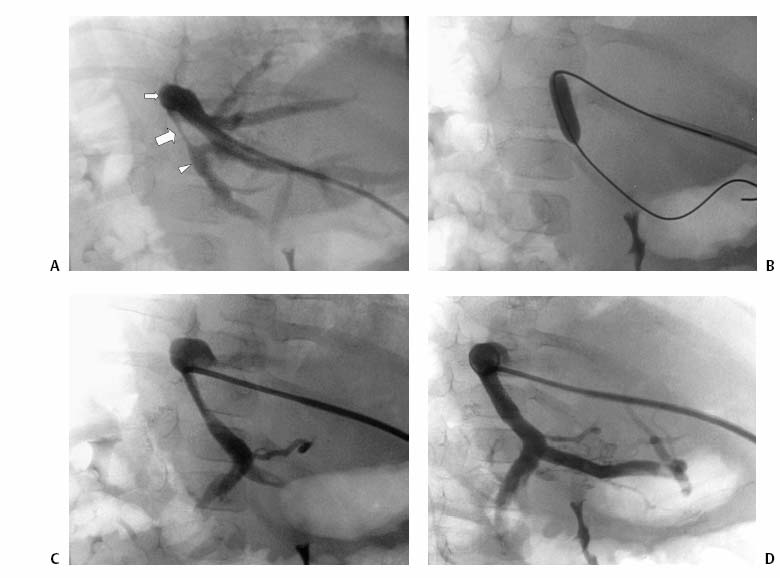
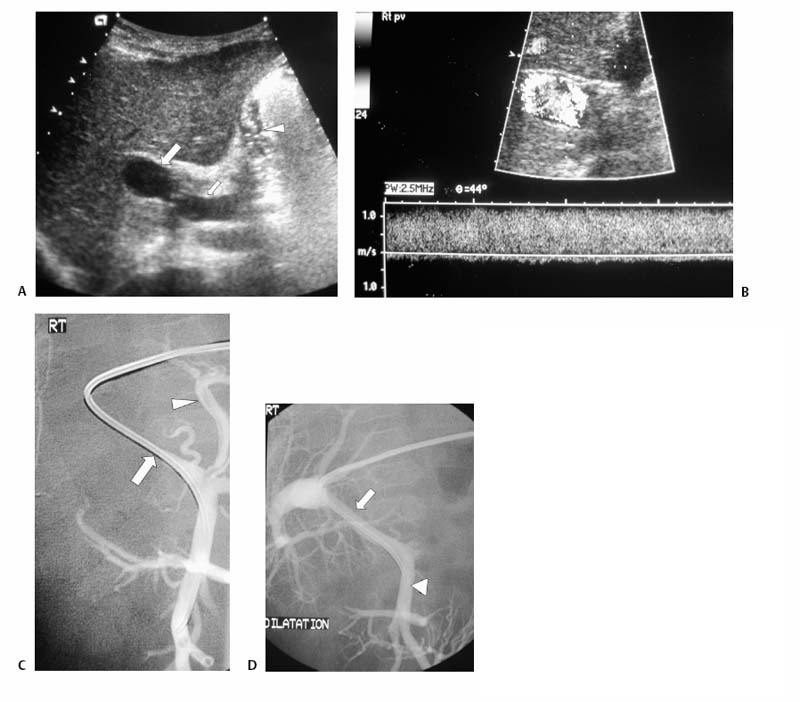
CASE 73 A 5-year-old male presented with abdominal distention 1 year after living-related liver transplantation. Figure 73-1 (A) A 5-year-old boy 1 year after living-related liver transplant. Transhepatic portal venography shows a left lateral segment liver transplant with a tight stenosis involving the length of the main portal vein (large arrow), between the donor intrahepatic portal veins (small arrow) and the recipient superior mesenteric vein (arrowhead). (B) Venoplasty of the venous anastomosis to 8 mm in diameter with complete resolution of the waist of the balloon. (C) Venogram shows recurrence indicating elastic stenosis. Despite multiple dilations, the stenosis persisted. A prominent coronary varix is opacified. (D) Venogram after successful stent placement shows complete resolution of the stenosis. Sonography with Doppler interrogation showed a left lateral segment graft, ascites, and a stricture involving the portal vein anastomosis with elevated flow velocity within the strictured segment. Transhepatic portal venography verified the tight stenosis (Fig. 73-1A). Portal vein stenosis complicating pediatric liver transplant. Under general anesthesia, the patient was placed in the supine position on the angiography table. From a subxyphoid approach using direct sonographic guidance, a portal vein branch of the left lateral segment was punctured using a 21-gauge needle (Micropuncture; Cook, Bloomington, Indiana). Exchange was made over a 0.018-inch wire for a 5-French (F) coaxial dilator. The coaxial dilator was exchanged over a standard 0.035-inch guidewire for a 5F Kumpe catheter (Cook, Bloomington, Indiana), and the wire and catheter were manipulated from the donor portal vein to the recipient superior mesenteric vein. Venography was performed with 4 cc of half-strength contrast material. A tight stricture of the portal vein was noted at the level of the portal venous anastomosis (Fig. 73-1A). Portal venous pressure measured 28 mm Hg on the recipient side and 8 mm Hg on the donor side of the stenosis, for a portosystemic gradient of 20 mm Hg. The Kumpe was replaced over a Rosen wire (Cook, Bloomington, Indiana) by a 7F vascular sheath, and a BlueMax balloon catheter (8-mm diameter, 2-cm length; Boston Scientific, Natick, Massachusetts) was used to dilate the stenotic segment (Fig. 73-1B). Complete resolution of the balloon waist was observed during inflation. Despite multiple balloon inflations, repeat venography showed only minimal improvement, indicating an elastic stenosis (Fig. 73-1C). A Wallstent (Boston Scientific, Natick, Massachusetts) was deployed, (8-mm diameter, 2-cm length), and venography showed complete resolution (Fig. 73-1D). The sheath was removed with deployment of Gelfoam pledgets (Pharmacia and Upjohn, Kalamazoo, Michigan) for tract embolization. The patient has been symptom-free during a follow-up period of 36 months. Contrast material Pressure transducer 5F Micropuncture set (Cook, Bloomington, Indiana) 15J guide wire (Cook, Bloomington, Indiana) Rosen wire (Cook, Bloomington, Indiana) 5F Kumpe catheter (Cook, Bloomington, Indiana) 7F vascular sheath (Cook, Bloomington, Indiana) Balloon catheter (8-mm diameter, 2-cm length) (Blue Max; Boston Scientific, Natick, Massachusetts) Wallstent (8-mm diameter, 2-cm length) (Boston Scientific, Natick, Massachusetts) Venous obstruction after pediatric liver transplantation can occur at the portal venous inflow as well as at the hepatic venous and inferior vena cava (IVC) outflow, and it has an overall incidence of approximately 8%. First-line treatment options include venoplasty and stent placement, with surgical reconstruction and retransplantation reserved for refractory cases. Portal vein obstruction may present variably with ascites, splenomegaly, elevated liver function tests, and, occasionally, variceal bleeding. Although portal vein obstruction may occur at the surgical anastomosis as a result of intimal hyperplasia, fibrosis, or surgical technique, the risk of this complication is increased with the use of cryopreserved venous conduits. In addition, in left lateral segment liver transplants, the stenosis often occurs as a result of kinking at the point of flexion of the extra-hepatic portal vein as it courses from right to left, anterior to the liver graft. Portal vein compression may increase as the liver grows. Sonography with Doppler is typically the first-line imaging modality for establishing the diagnosis (Fig. 73-2).
Clinical Presentation
Radiologic Studies
Diagnosis
Treatment
Equipment
Discussion
Background
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree