Diagnosis: Atypical femoral insufficiency fracture in a patient on bisphosphonate therapy
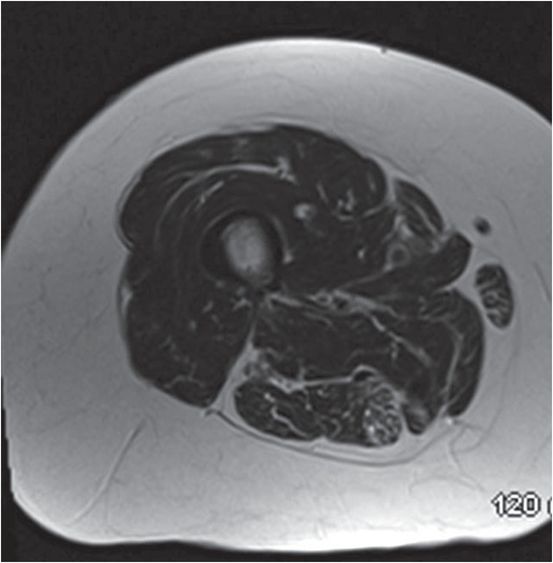
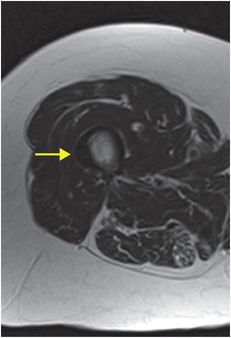
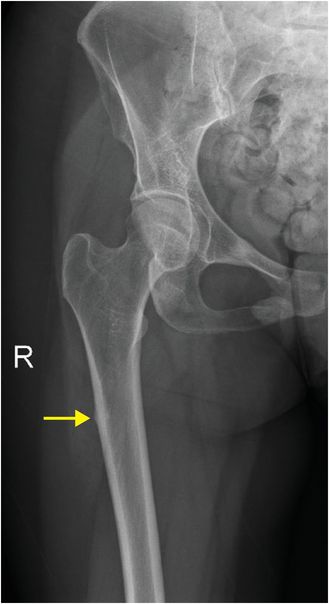
Frontal radiograph of the right femur demonstrates focal cortical thickening along the lateral aspect of the proximal femoral diaphysis (arrow). Coronal STIR MR (middle image) demonstrates focal increased fluid signal along the lateral diaphyseal cortex (arrow). Axial T1-weighted image demonstrates focal cortical thickening laterally (arrow). Case courtesy Ketan I. Patel, MD.


Discussion
Patients with fractures associated with long-term bisphosphonate use often report vague thigh pain with minimal or no trauma history.
The proximal femur is exposed to substantial impact from normal activity on a daily basis; fracture of this normally strong bone in the absence of high-energy trauma is due to an underlying bone abnormality (insufficiency fracture, defined by normal stress on an abnormal bone).
Abnormal bone remodeling from prolonged osteoclast suppression is the theorized cause of bisphosphonate-associated fractures.
Imaging of bisphosphonate-associated insufficiency fracture may be subtle.
Radiographic findings include focal cortical thickening and transverse lucency through the lateral cortex (up to 98% specific). Findings may be very subtle, as in the index case. Fractures are usually close to the lesser trochanter. When complete, there may be a sharp medial projection or “medial spike”, usually associated with the distal fragment, where the fracture line transitions steeply from horizontal to vertical. Comminution is unusual.
In contrast to insufficiency fractures, fatigue fractures occur with abnormal stress on normal bone. These fractures tend to affect younger athletes rather than elderly patients with osteoporosis, and usually involve the medial rather than lateral cortex.
Clinical management of bisphosphonate-associated insufficiency fracture varies depending on clinical and radiographic findings.
Bisphosphonate-associated fractures are often bilateral, and therefore, it is advisable to obtain radiographs of the contralateral femur to assess for clinically silent fractures when one is diagnosed.
Management options include discontinuation of bisphosphonates, trial of non-weight bearing, and prophylactic placement of an intramedullary fixation rod. Many orthopedic surgeons recommend prophylactic fixation of nondisplaced bisphosphonate-associated fractures, as progression to displacement is common and generally results in increased pain, morbidity, and cost to the patient.
Specific findings such as thickening of the lateral cortex, predominantly transverse orientation of the fracture line, and medial spike should be sought in all cases of subtrochanteric fracture in susceptible populations (elderly patients, patients with malignancy, etc.).
Clinical synopsis
The patient underwent prophylactic intramedullary femoral rod placement and discontinuation of bisphosphonate therapy.
Self-assessment
|
|
|
|
Spectrum of bisphosphonate-associated insufficiency fracture
Progression from nondisplaced to complete fracture
In this case of bisphosphonate-associated insufficiency fracture, an initial radiograph (upper image) demonstrated subtle cortical thickening of the lateral cortex in the subtrochanteric femur (yellow arrow). Ongoing weight bearing ultimately resulted in complete transverse fracture at the same site, as seen on the follow-up image taken when the patient presented with acute pain. The distal fracture fragment has a medial spike (red arrow), which is characteristic of a bisphosphonate-associated insufficiency fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree