8 SPECT and SPECT/CT for the Skeletal System
8.1 Introduction
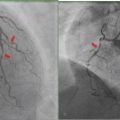
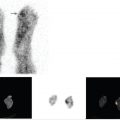
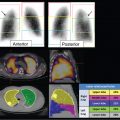
Skeletal scintigraphy is one of the most commonly requested general nuclear medicine studies due to its wide availability, ease of performance, low cost, and ability to assess the entire skeletal system. Often, abnormalities can be identified on skeletal scintigraphy earlier than on anatomical imaging. Since radiotracer uptake in the skeleton occurs as a result of osteoblastic activity, it can be seen in traumatic, infectious, and neoplastic conditions. Thus, although the sensitivity of skeletal scintigraphy is high, correlation with clinical history and additional imaging is crucial for accurate image interpretation (► Fig. 8.1). Single-photon emission computed tomography (SPECT; ► Fig. 8.2) and SPECT/computed tomography (SPECT/CT; ► Fig. 8.3) can improve image contrast as well as cross-sectional anatomical detail, resulting in higher sensitivity, specificity, diagnostic accuracy, and reader confidence compared with planar skeletal scintigraphy alone.



Although adding CT to SPECT increases the radiation dose to the patient, the benefits often far outweigh the risks associated with the additional radiation exposure. The CT data can be used for attenuation and scatter correction, thus improving the quality of SPECT. The addition of CT has allowed us to clarify SPECT findings and has also increased our ability to determine the anatomical location and extent of disease and enabled concurrent evaluation of anatomical and metabolic changes, thereby assisting with surgical planning and determination of appropriate management. Today, some of the most common indications for skeletal scintigraphy with SPECT or SPECT/CT include evaluation of suspected radiographically occult fractures and stress changes; postsurgical complications, such as pain and hardware instability; and suspected neoplastic disease. Skeletal scintigraphy with SPECT or SPECT/CT is also often used when magnetic resonance imaging (MRI) cannot be performed because of contraindications or a high likelihood of artifact.
8.1.1 Technique
Bone is made up of a crystalline lattice consisting of calcium, phosphate, and hydroxyl ions that form hydroxyapatite. Bone-targeting radiopharmaceuticals are analogues of calcium, hydroxyl groups, or phosphates and are taken up in osteoblasts at the time of bone remodeling or healing. 1 Among them, technetium-99 m (99mTc)-labeled methylene diphosphonate (MDP) is the most widely used radiopharmaceutical for skeletal scintigraphy. Images are typically acquired as either a single- or a three-phase study. No patient preparation is required prior to the study.
In a three-phase bone scan, angiographic phase (blood flow) images are acquired by dynamic imaging, usually for 60 seconds, immediately after the injection of 740 to 925 MBq (20-25 mCi) of 99mTc-MDP to assess perfusion to the area of interest. Tissue phase (blood pool) static images are acquired once the dynamic imaging has been completed and are used to assess hyperemia or the amount of activity that extravasates into the soft tissue in the area of interest. Skeletal phase imaging is performed 2 to 4 hours afterward to assess skeletal uptake. Three-phase bone scans are often done to evaluate traumatic injury where knowledge regarding perfusion is needed, such as in cases of suspected complex regional pain syndrome or osteomyelitis. They are also useful for the evaluation of neoplastic osseous disease, such as for a suspected osteoid osteoma, among other pathologies.
In a single-phase bone scan, only skeletal phase imaging is performed. Single-phase bone scans are commonly done for follow-up of patients with known osseous metastases.
SPECT or SPECT/CT is obtained at the time of skeletal phase imaging as needed and is usually targeted to a site of abnormality on planar images or to improve the sensitivity and specificity in a region of clinical concern. SPECT is typically acquired using a 128 x 128 matrix with 25 seconds per step, iterative reconstruction, and resolution recovery. Images are displayed in coronal, sagittal, and axial projections alongside a rotating maximum intensity projection (MIP) image. For the CT portion of the study, the typical kVp range is 80 to 110 kVp and slice thickness is 2 to 2.5 mm with overlapping cuts; however, the CT may be tailored to the clinical question, varying from very low dose for attenuation correction, to low dose for anatomical correlation, to normal dose for more precise anatomical imaging when needed. Intravenous contrast administration is not performed, and dose modulation is applied to minimize radiation exposure. Also, radiation exposure can be minimized by avoiding the use of CT when unlikely to provide additional value to SPECT. Bone and soft tissue windows as well as reformats in coronal and sagittal projections are available for studies with three-dimensional rendering as required. Fused and nonfused SPECT and CT images are reviewed. Since CT images are rapidly acquired (in a matter of seconds), motion is rarely an issue. SPECT typically requires 12 to 15 minutes to complete and can lead to potential misregistration artifact between the CT and SPECT images. Thus it is important to ensure that patients are comfortably positioned whenever possible.
8.1.2 Pearls
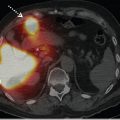
Intense activity in the bladder can cause artifact on reconstructed SPECT images, including streak artifact and “cold” areas close to the bladder due to pixel overload (► Fig. 8.4). Therefore, if the patient cannot void and there is clinical concern for sacral, pelvic bone, or proximal femoral abnormality, bladder catheterization may be helpful.

8.2 Trauma/Arthropathy/Unexplained Pain
Skeletal scintigraphy has long been used for the evaluation of traumatic injury, and there are a number of indications as to when SPECT or SPECT/ CT should be considered. In particular, SPECT or SPECT/CT can be particularly useful (1) to diagnose a clinically suspected fracture in the setting of negative anatomical imaging, (2) to diagnose a cause of mechanical back pain or pars stress, and (3) for the evaluation of pain after surgical intervention when MRI is subject to significant artifact. Whole-body skeletal scintigraphy with additional SPECT or SPECT/CT where needed is also good to provide a rapid whole-body assessment with limited radiation exposure for the detection of multifocal traumatic injury that may be difficult to obtain using anatomical imaging modalities, such as radiographs, CT, or MRI.
8.2.1 Fractures
Skeletal scintigraphy with SPECT or SPECT/CT is helpful in patients with pain, a clinical history of trauma or osseous stress, and negative diagnostic imaging. Stress injury occurs following repetitive activity causing marrow edema and microtrabecular fractures that ultimately coalesce to form a cortical break. Skeletal scintigraphy is exquisitely sensitive for stress injury and fractures. Indeed, active osteoblastic turnover can be seen prior to anatomical changes and often correlates with the site of pain. 2 , 3 SPECT/CT has improved diagnostic accuracy compared with planar imaging alone or with SPECT and can be particularly helpful to localize abnormalities in patients with radiographically occult stress fractures (► Fig. 8.5) or osteochondral defects (► Fig. 8.6). Linke et al studied 71 patients with extremity pain and found that planar imaging and SPECT/CT led to a different diagnosis compared with planar imaging and SPECT in 23 patients (p <0.01). 4 Scheyerer et al found improved diagnosis of occult pelvic fractures on SPECT/CT compared with radiographs and CT, 5 while Allainmat et al found improved diagnosis of occult wrist fractures on SPECT/CT compared with CT. 6 MRI is sensitive for bone marrow edema; however, the extent of edema is protocol dependent, and image interpretation can be difficult and/ or misleading. Skeletal scintigraphy with SPECT or SPECT/CT can also identify ongoing active osteoblastic turnover, which can be useful to suggest when healing is complete as well as the presence of nonunion. Active osteoblastic turnover 12 to 18 months after a fracture is suggestive of nonunion. 2


8.2.2 Back Pain
SPECT or SPECT/CT is recommended for the evaluation of back pain. SPECT has been shown to have improved specificity compared with planar skeletal scintigraphy, particularly for the evaluation of lesions in the lumbar spine. 7 , 8 CT increases the specificity still further. 9 Moderately to markedly active facet arthropathy is generally evident on planar images, demonstrating a characteristic appearance. 10 However, mild facet arthropathy may not be apparent on planar images, while it is clearly evident on SPECT or SPECT/CT (► Fig. 8.7). Skeletal scintigraphy with SPECT or SPECT/CT may also be helpful to identify active osteoblastic turnover at sites of pain associated with transitional vertebra or stress to the region of the pars interarticularis. 2

8.2.3 Accessory Ossicles
Skeletal scintigraphy with SPECT/CT may be helpful to precisely localize the site of active osteoblastic turnover to an accessory ossicle. Active osteoblastic turnover associated with an accessory ossicle may suggest a cause of pain (stress, fracture, inflammation, etc.) versus absent activity, which is more commonly associated with a normal anatomical variant, an important distinction if surgical resection is considered. 2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree