Diagnosis: Lisfranc fracture–dislocation, homolateral type
Frontal and oblique radiographs of the right foot demonstrate a comminuted fracture through the base of the second proximal metatarsal (yellow arrows). There is widening and distortion of the Lisfranc joint (red arrow), with lateral displacement of all metatarsals including the first, consistent with homolateral injury.


Discussion
The Lisfranc joint complex is comprised of tarsometatarsal (TMT), intermetatarsal, and intertarsal articulations, as well as ligaments including the Lisfranc, plantar tarsometatarsal, dorsal tarsometatarsal, and intermetatarsal ligaments, which are not routinely distinguished at MR imaging
The Lisfranc ligament extends from the medial cuneiform to the base of the second metatarsal, and is divided into dorsal, interosseous, and plantar components, with the plantar component being the most important.
Normal Lisfranc ligament: Axial T1-weighted MR (left image) and T2-weighted MR with fat saturation depict the normal Lisfranc ligament connecting the medial cuneiform to the base of the second metatarsal (arrows). Note the normal very low signal of the ligament on both sequences without associated edema.


Lisfranc ligament sprains generally result from low-impact midfoot injury, while Lisfranc fracture–dislocations result from high-impact injury.
These injuries account for 0.2% of all fractures and less than 1% of all dislocations.
Delayed recognition leads to chronic pain, significant functional loss, and osteoarthritis.
Common mechanisms of Lisfranc injury include direct trauma (such as crush injury) and indirect trauma (such as forced plantar flexion and forefoot abduction).
Common clinical symptoms include pain at the TMT joint of the midfoot and inability to bear weight. Limited forefoot abduction or adduction, plantar ecchymosis, and shortening of the foot are less common presenting features.
There are two types of dislocation in Lisfranc injury.
Homolateral dislocation is defined as lateral displacement of the first through fifth metatarsals.
Divergent dislocation is defined as medial dislocation of the first metatarsal with lateral dislocation of the second through fifth metatarsals.
Most common fractures associated with Lisfranc injury involve the medial aspect of the second metatarsal base or the distal lateral aspect of the medial cuneiform.
On radiography, more than 2 mm of separation between first and second metatarsal on weight-bearing views suggests Lisfranc ligament tear, while frank displacement of the second metatarsal and medial cuneiform is suggestive of complete tear.
On radiography or MR, nonalignment of the lateral aspect of the first metatarsal and medial cuneiform and the medial aspect of the fourth metatarsal and cuboid suggest a Lisfranc injury.
As many as 20% of Lisfranc joint injuries are estimated to be missed on conventional non-weight-bearing AP and lateral radiographs. CT is highly sensitive for identifying fractures not identified on plain radiographs or MR.
MR findings of Lisfranc injury include abnormal signal (i.e., sprain) or frank disruption (i.e., tear) of the Lisfranc ligament, malalignment of the dorsal arch, TMT joint subchondral edema suggestive of avulsion fracture, and marrow edema within the metatarsals or medial and middle cuneiforms.
Clinical synopsis
The patient underwent open reduction and internal fixation with arthrodesis of the first, second, and third TMT joints.
Self-assessment
|
|
|
|
|
|
Spectrum of Lisfranc injuries
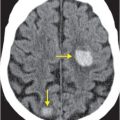
Lisfranc fracture–dislocation, homolateral type
Frontal and oblique radiographs demonstrate a tiny osseous fragment adjacent to the lateral aspect of the medial cuneiform (known as the “fleck sign”; yellow arrow), and offset at the second TMT joint (red arrows), best appreciated on the oblique view. Open reduction and plate and screw internal fixation was performed. Displacement of the second metatarsal and lateral shift of the base of the first metatarsal was noted during surgery, consistent with a homolateral type injury.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree