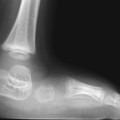
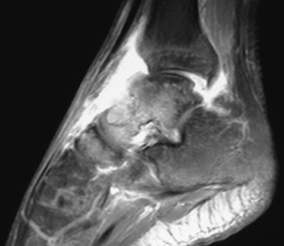
CASE 90 A 17-year-old presents with an acutely swollen tender ankle. Figure 90B Figure 90B Lateral radiograph demonstrates evidence of a tibiotalar joint effusion with a large erosion showing marginal indistinct sclerosis at the talar neck (Fig. 90A). Corresponding sagittal fat-suppressed enhanced T1-weighted MRI depicts a joint effusion with diffuse increased signal intensity within talus and navicular (Fig. 90B). There is a focal area of higher signal intensity with a low-intensity margin within the talar neck with loss of adjacent anterior cortex. Septic arthritis Septic arthritis, defined clinically as joint inflammation, is an infection of the joint space. It is diagnosed with a positive synovial or blood culture, an antigen detection test, or a standard tube agglutination titer of 160 or greater for Brucella species. Approximately 7% of childhood arthritis is septic in origin with the vast majority of these patients being previously healthy. The incidence varies with age (ranging from 5 to 37 per 100,000), being most common in patients <2 years old (one third to one half of cases). Septic arthritis is most commonly seen in the hip and knee joints, followed by ankle and shoulder. Hematogenous seeding during a bacteremic episode is the most common etiology in children. Less commonly, the infectious joint is the result of direct extension from an adjacent cellulitis/myositis. Spread from an adjacent osteomyelitis is seen more often in infants <8 months or >18 months of age, particularly in the hip, where the physis is intra-articular. Traumatic penetration of the joint is a less common etiology but can be seen with plant-thorn synovitis.
Clinical Presentation

Radiographic Findings
Diagnosis
Differential Diagnosis
Discussion
Background
Etiology
Clinical Findings
Complications
Pathophysiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree