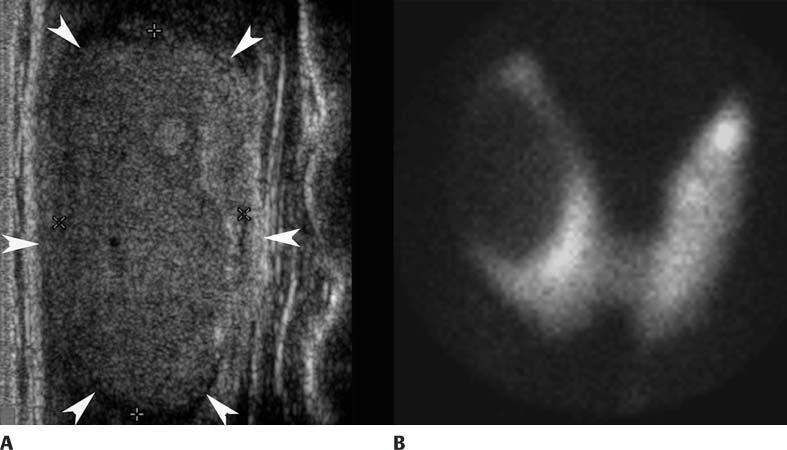
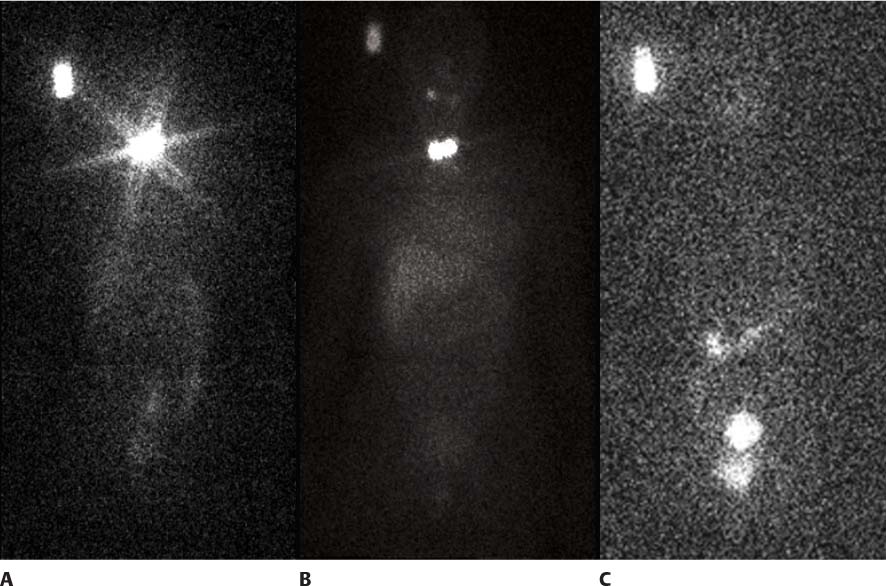
CASE 98 A 34-year-old woman presents with a lump in her neck (Figs. 98.1). Fig. 98.1 Fig. 98.2 • 99mTc-pertechnetate, 10 mCi (370 MBq) intravenously. Planar imaging of the neck with a pinhole collimator 20 minutes later (Fig. 98.1B). • 131I, 2 mCi (74 MBq) orally. Planar imaging with a high-energy collimator 2 days later (Fig. 98.2A, C). • 131I, 100 mCi (3700 MBq) orally (therapy dose). Planar imaging with a high-energy collimator 7 days later (Fig. 98.2B). Coronal image from thyroid ultrasound (Fig. 98.1A) reveals a 3.5-cm mildly heterogeneous nodule (arrowheads) in the right lobe. 99mTC scan (Fig. 98.1B) demonstrates very little uptake in the nodule (“cold” nodule). The incidence of malignancy in cold nodules is 15 to 20%, so a fine-needle aspiration biopsy is performed, diagnosing papillary thyroid cancer. The patient undergoes thyroidectomy and is referred to nuclear medicine for therapy with 131I. A pre-therapy scan is performed (Fig. 98.2A) 2 days following the oral administration of 131I, 2 mCi. As expected, there is intense uptake in the thyroid remnant, resulting in some star artifact as a result of collimator penetration. There is physiologic uptake in the liver, bowel, and bladder, with no evidence of iodine-avid metastases. A rectangular area of activity to the right of the head is within a standard of known activity placed next to the patient for calculation purposes. A 100 mCi oral dose of 131I was administered for therapy purposes without incident. The patient returned 1 week later for a post-therapy scan with the on-board therapy dose of 131I (Fig. 98.2B). This confirmed the absence of metastases. A follow-up diagnostic scan (2 mCi) 6 months later (Fig. 98.2C) demonstrates successful ablation of the thyroid remnants and no metastases; there is physiologic up-take in the colon, bladder, and (mild uptake) in salivary glands.
Clinical Presentation
Technique
Image Interpretation
Therapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree