Case presentation
A 6-month-old baby with cough, congestion, and fever for 3 days presents to the emergency department with complaints of respiratory distress. Physical examination is significant for a temperature of 102 degrees Fahrenheit, respiratory rate of 55 breaths per minute, pulse oxygen saturation of 92%, and prominent intercostal, subcostal, and suprasternal retractions. On auscultation, there are diffuse crackles and intermittent wheezing heard in all lung fields. Mucous membranes are moist, and the child is still alert and playful despite increased work of breathing.
Imaging considerations
Several studies have shown that the routine use of radiographs in children with mild bronchiolitis or classic illness may lead to inappropriate antibiotics and is currently not recommended for routine use by pediatric practice guidelines. Secondary bacterial pneumonia is an uncommon complication and should be considered in children not having the expected clinical course or those admitted to the intensive care unit (ICU).
Radiographs are most likely to be useful in children with focal findings, severe disease, or signs of complications such as pneumothorax or when history and physical examination point to other causes in the differential diagnosis that may mimic aspects of the bronchiolitis examination (i.e., undiagnosed heart disease, myocarditis, foreign body, etc.).
Plain radiography
The most common radiographic findings in bronchiolitis are either normal radiographs or a combination of findings that often include peribronchial thickening, hyperinflation, and atelectasis. Radiographs are ideal to detect complications such as pneumothorax or bacterial co-infection in children who do not have clinical signs of classic bronchiolitis.
Thoracic ultrasound (US)
Smaller studies have looked at the use of lung US scans in the inpatient settings in correlation with clinical examination findings in investigating for pneumonia. The presence of B lines, subpleural consolidations, and interstitial disease along multiple spaces has been attributed to more severe disease and bacterial pneumonia. However, interrater reliability, operator variability, and lack of validation to differentiate viral versus bacterial disease in these small studies limit the use of US on a broader scale for most cases. ,
Imaging findings
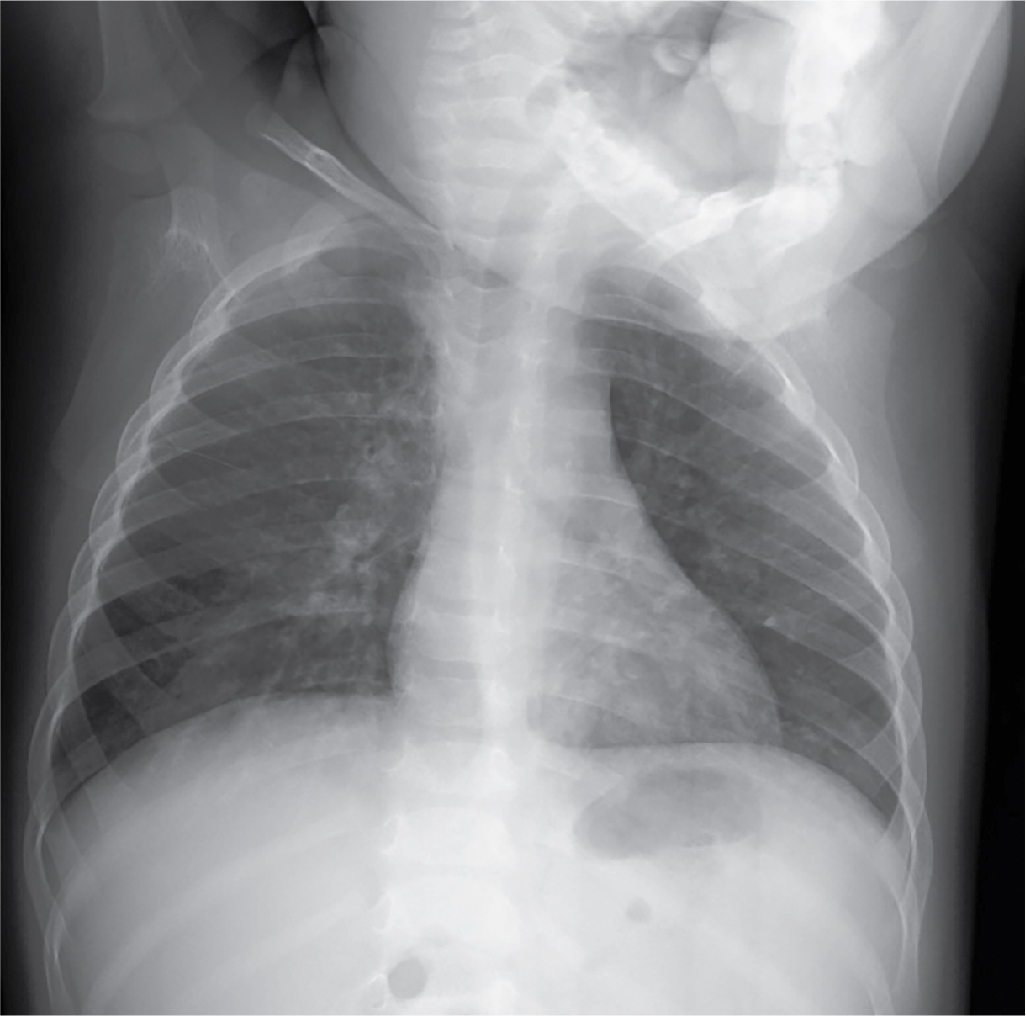
This child had imaging performed by his primary care provider earlier in the day. A two-view chest radiograph study is shown. There are bilateral patchy and streaky perihilar opacities, diffuse interstitial prominence, and central airway thickening. There is no focal infiltrate or effusion, including the retrocardiac space ( Figs. 5.1 and 5.2 ). Similar imaging findings for a different child with bronchiolitis are also shown ( Figs. 5.3 and 5.4 ).