Case presentation
A 5-day-old male infant presents with decreased feeding and activity for the past 24 hours. The parents report emesis that initially looked like infant formula but over the past 12 hours has become “yellow-green” and the last several episodes have been “green.” The emesis has occurred whenever the child attempts to feed, which was typically every 3 hours, but the parents have been attempting to feed more frequently (every hour or so) because they feel the child is not “keeping anything down.” There has been no fever, cough, congestion, rhinorrhea, or reported/known trauma. The child had initially been fussy and appeared “uncomfortable.”
The child’s physical examination reveals an ill-appearing, afebrile child. His heart rate is 116 beats per minute, respiratory rate is 20 breaths per minute, and oxygen saturations are 96% on room air. He has a sunken anterior fontanelle, dry mucous membranes, and dry skin without lesions. His skin turgor is poor with delayed capillary refill. There is no appreciable heart murmur and his lungs are clear. His abdominal examination demonstrates generalized distention with no obvious hepatosplenomegaly and the abdomen appears to be tense.
Imaging considerations
Emesis in the neonate has causes that range from benign to life-threatening, and history and physical examination can help to determine the need for imaging. Bilious emesis can indicate a surgical emergency and, while imaging is desirable, rapid treatment of the patient and prompt surgical consultation should not be delayed in these patients, especially if they appear ill or are in extremis.
Plain radiography
Plain abdominal radiography is a readily available imaging modality and can provide the clinician with an overall view of the bowel gas pattern, as well as the presence of pneumoperitoneum. This is a first-line imaging modality when intestinal pathology is suspected, such as bowel obstruction, and may demonstrate gaseous distention of the stomach and proximal duodenum when a volvulus is present. However, children with malrotation often have a normal bowel gas pattern.
Fluoroscopy
Upper gastrointestinal series (UGI) is the imaging study of choice for the diagnosis of malrotation. UGI has a sensitivity of 93% to 100% for malrotation, , and studies have found a positive predictive value of 90%. Patients with malrotation will have an abnormal position of the duodenojejunal junction and there are a variety of abnormal positions that are associated with malrotation. If Ladd bands are present, abnormal duodenal configuration may be noted, and if there is midgut volvulus, a corkscrew pattern and possible obstruction of the duodenum may be seen. , , , The reported sensitivity of UGI for detecting volvulus is 79%. , Anatomic variants can interfere with proper interpretation of a UGI series and special attention should be given to proper technique to ensure a meaningful study. , , This imaging test should be performed and interpreted by a pediatric radiologist or a radiologist experienced in pediatric fluoroscopy. If this expertise is not available, the clinician should arrange transfer of the patient to a facility that has this capability.
Ultrasound (US)
The role that US plays in the diagnosis of intestinal malrotation and volvulus is a matter of debate. While large studies are lacking, there is evidence to suggest that ultrasonography is useful in detecting malrotation. A finding described as suggestive of malrotation is inversion of the usual relationship of the superior mesenteric artery (SMA) and the superior mesenteric vein (SMV). Although some have reported this SMA/SMV inversion to be sensitive in detecting malrotation, both false-positive and false-negative results in studies have been reported. , An abnormal relationship between the SMA and the third segment of the duodenum on US has also been utilized to detect malrotation, and the presence of a “whirlpool sign” (a swirling appearance of the mesentery and SMV around the SMA) is suggestive of volvulus. , , This latter finding should prompt either confirmatory UGI or surgical consultation. , , , When combining these three sonographic features (inversion of the SMA and SMV, the whirlpool sign, and an intraperitoneal transverse duodenum), Zhou et al. found a sensitivity of 100% and specificity of 97.8%, noting that the study included 70 children with a mean age of 31 days. The prospect of utilizing US as a means to identifying malrotation is an exciting one, but additional study is needed before this modality is considered as a first-line test or as a replacement to a UGI. Also, US examination for these vascular and intestinal relationships is operator dependent and likely to have greatest utility in facilities with dedicated pediatric sonographers and pediatric imagers, rather than in a general community setting.
Computed tomography
This modality is not a first-line imaging test and is typically not employed when investigating malrotation or volvulus. It can differentiate between malrotation and nonrotation and may detect malrotation when the study is employed for other clinical reasons.
Magnetic resonance imaging (MRI)
MRI is not a first-line imaging modality when assessing for the presence of intestinal malrotation but can detect this condition. In a pediatric study of MRI compared to UGI, the authors found that if four specific anatomic criteria were met by MRI, then intestinal rotation could be considered normal. While MRI has the potential to avoid ionizing radiation exposure, it is not the gold standard at this time and, if performed, is an ancillary study.
Imaging findings
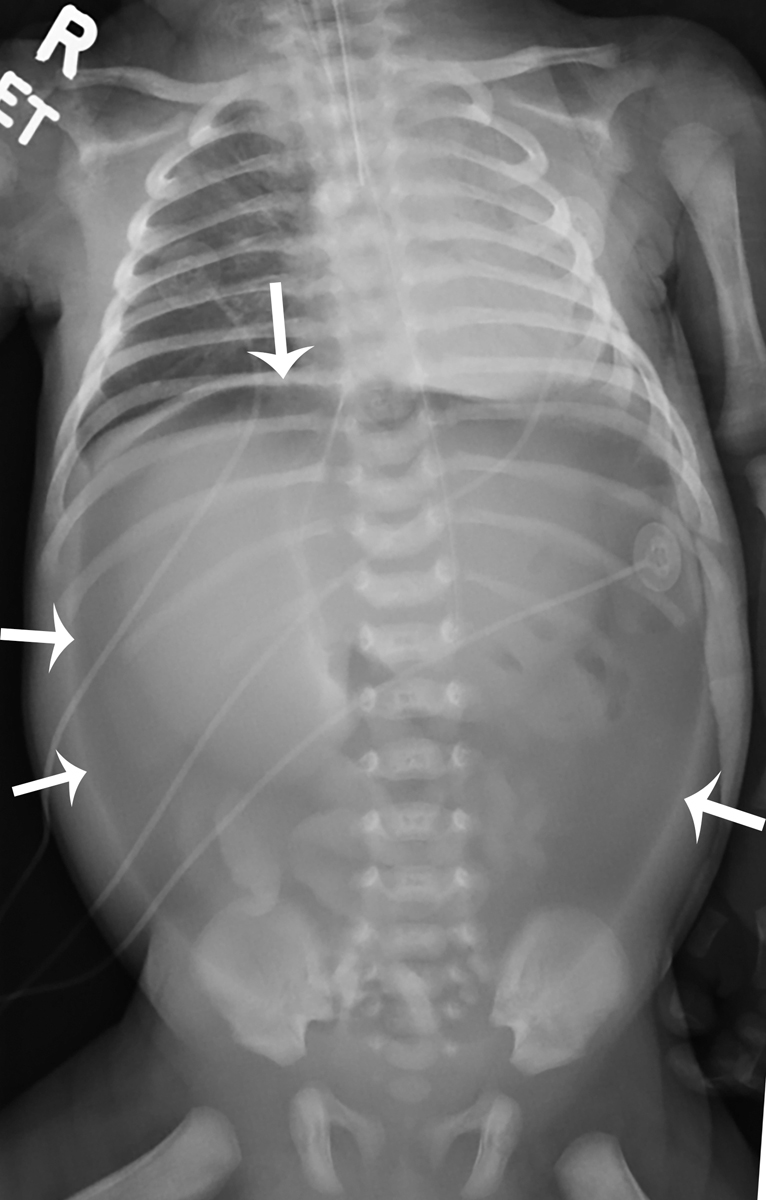
The child was thought not to be stable enough to undergo a UGI. Plain bedside radiography was obtained, as initial resuscitation began and the patient was intubated. Postintubation imaging, including one-view chest imaging and two-view abdominal imaging, was provided. There was a large pneumoperitoneum; the tip of the endotracheal tube was seen just above the carina but retracted into the midthoracic trachea and there was a nasogastric tube in the stomach ( Figs. 6.1 and 6.2 ).