Breast MR imaging is the most sensitive imaging method for the detection of breast cancer and detects more aggressive malignancies than mammography and ultrasound examination. Despite these advantages, breast MR imaging has low use rates for breast cancer screening. Abbreviated breast MR imaging, in which a limited number of breast imaging sequences are obtained, has been proposed as a way to solve cost and patient tolerance issues while preserving the high cancer detection rate of breast MR imaging. This review discusses abbreviated breast MR imaging, including protocols, multicenter clinical trial results, clinical workflow implementation challenges, and future directions.
Key points
- •
Studies have demonstrated that abbreviated breast MR imaging diagnostic accuracy and sensitivity for breast cancer detection is comparable with that of a full diagnostic protocol in screening populations.
- •
Abbreviated breast MR imaging protocols remain under development, but include, at a minimum, precontrast and postcontrast T1-weighted images.
- •
Current limitations of abbreviated breast MR imaging include nonscreening applications and the evaluation of invasive lobular carcinomas and low-grade ductal carcinoma in situ.
- •
Clinical implementation challenges include the current lack of Current Procedural Terminology coding and minimizing turnaround time as well as imaging time.
- •
Future directions include the implementation of ultrafast and multiparametric protocols.
Introduction
Breast MR imaging is the most sensitive imaging method for the detection of breast cancer. , Although mammography remains the gold standard for breast cancer screening, numerous high-quality multicenter trials have demonstrated that breast MR imaging detects on average 3 to 4 times as many breast cancers as mammography in patients with a high (>20%–25%) lifetime risk of breast cancer, with cancer detection rates ranging from 14.7 to 16.0 per 1000 women (compared with 5.1 per 1000 women in screening mammography). Although traditionally breast MR imaging has been offered as supplemental screening for high-risk women only, increased cancer detection rates with breast MR imaging have been demonstrated in patients with intermediate (15%–20%) lifetime risk , and even average (<15%) lifetime risk of breast cancer.
Breast MR imaging offers superior cancer detection to screening mammography and ultrasound examination owing to the uptake of gadolinium intravenous contrast and improved tissue contrast. These features of MR imaging allow for the evaluation of real-time, functional wash-in and wash-out of contrast within the breast parenchyma. The increased angiogenesis and vessel permeability in invasive breast cancer results in avid uptake of contrast compared with the background parenchymal enhancement. Early uptake of contrast has also been demonstrated in high-grade ductal carcinoma in situ (DCIS), which may reflect pathologically increased permeability of the ductal membrane in higher grade DCIS owing to protease activity. The physiologic uptake of contrast in high-grade DCIS and invasive cancers explains the increased detection of these more aggressive malignancies on MR imaging when compared with mammography and ultrasound examination.
Despite the clear advantages of breast MR imaging, it is traditionally recommended only to patients who have a high lifetime breast cancer risk. Recent guidelines have suggested a benefit for women an intermediate lifetime risk as well. Despite these recommendations, only 1.5% of women with a high lifetime risk in the community have ever had a breast MR imaging. This low use likely primarily reflects the traditional high cost of this examination, with cost-effectiveness studies previously showing maximum usefulness in high-risk patients. Other factors often cited in the low use of breast MR imaging include patient tolerance, accessibility, and patient claustrophobia. ,
Abbreviated breast MR imaging, in which a limited number of breast imaging sequences are obtained, has been proposed as a way to solve both cost and patient tolerance issues while preserving the high cancer detection rate of breast MR imaging. Numerous studies have shown that abbreviated breast MR imaging screening can considerably decrease table time and reading time compared with a full breast MR imaging, while offering the same high positive predictive value and diagnostic accuracy. The recent Eastern Cooperative Oncology Group-American College of Radiology Imaging Network EA1141 multicenter trial has offered the first proof of the increased cancer detection rate of abbreviated breast MR imaging in average risk patients compared with digital breast tomosynthesis (DBT), paving the way for wider adoption of this screening method.
The purpose of this review is to discuss (1) the background of abbreviated MR imaging, (2) the various proposed abbreviated MR imaging protocols, (3) the known limitations of the modality, and (4) the challenges of clinical implementation.
Imaging technique
Abbreviated breast MR imaging was first described by Kuhl and colleagues in 2014. In this landmark work, Kuhl and colleagues evaluated 443 women with average to intermediate lifetime risk in a series of 606 screening MR imaging and demonstrated that the diagnostic accuracy and positive predictive value were equivalent between an abbreviated protocol and a full breast imaging protocol. Kuhl’s protocol included a noncontrast T1-weighted and a single postcontrast T1-weighted sequence, with generated subtraction images (first postcontrast acquisition subtracted [FAST]) and maximum intensity projection (MIP) images. The average imaging time was 3 minutes compared with a full protocol time of 17 minutes table time; interpretation time was 28 seconds for the FAST images. Although Kuhl’s protocol consists of the stripped-down essentials for an abbreviated protocol, multiple iterations have been subsequently proposed ( Table 1 ).
| Reference | Ultrafast | Standard Temporal Resolution | Sens | Spec | Max Area Under the Curve | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-T1W | FAST T1W | Second/Delayed Post T1W | T2W | Sub | MIP | |||||
| Platel et al, 2014 | Y | Y | Y | N | N | Y | Y | NA | NA | 0.87 |
| Kuhl et al, 2014 | N | Y | Y | N | N | Y | Y | 100% | 94.3% | NA |
| Mann et al, 2014 | Y | N | N | N | N | N | N | 90% | 67% | 0.812 |
| Mango et al, 2015 | N | Y | Y | N | N | Y | Y | 93%–98% | NA | NA |
| Grimm et al, 2015 | N | Y | Y | Y | Y | Y | N | 86%–89% | 45%–52% | NA |
| Harvey et al, 2016 | N | Y | Y | N | N | Y | Y | 100% | 94% | NA |
| Heacock et al, 2016 | N | Y | Y | N | Y | Y | N | 97.8%–99.4% | NA | NA |
| Moschetta et al, 2016 | N | Y | Y | N | Y | Y | Y | 89% | 91% | NA |
| Abe et al, 2016 | Y | Y | Y | N | N | Y | N | 85% | 79% | 0.89 |
| Machida et al, 2017 | Y | Y | Y | N | N | N | N | 87.1%–93.5% | 83.4%–91.7% | NA |
| Chen et al, 2017 | N | Y | Y | N | N | Y | Y | 92.9%–93.8% | 86.5%–88.3% | NA |
| Petrillo et al, 2017 | N | Y | Y | N | N | Y | Y | 99.5% | 75.4% | NA |
| Panigrahi et al, 2017 | N | Y | Y | N | N | Y | Y | 81.8% | 97.2% | NA |
| Romeo et al, 2017 | N | Y | Y | N | Y | Y | N | 99% | 93% | NA |
| Oldrini et al, 2017 | Y | Y | Y | N | Y | Y | N | 93.1% | 70.8%–83.3% | NA |
| Choi et al, 2017 | N | Y | Y | N | Y | Y | Y | 100% | 89.2% | NA |
| Oldrini et al, 2018 | N | Y | Y | N | N | Y | N | 100% | 95.1% | NA |
| Lee-Felker et al, 2019 | N | Y | Y | N | N | Y | Y | 99% | 97% | NA |
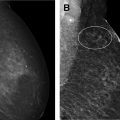
This initial abbreviated protocol can be compared with the American College of Radiology accreditation requirements for breast MR imaging, which include a scout localizer, T2-weighted images and precontrast and postcontrast T1-weighted images. Postcontrast images must include both early and delayed images; generally, at least 3 postcontrast series are acquired. Postprocessing often includes subtraction and MIP images. Additional specialized sequences may include diffusion weighted imaging (DWI), ultrafast (<10 second temporal resolution), and other multiparametric imaging sequences. For this full MR protocol, average table time is approximately 17 to 35 minutes, and this is generally scheduled in a 30- to 60-minute time slot ( Fig. 1 ).

Screening protocol literature
Overview
Since Kuhl and colleagues first evaluated abbreviated breast MR imaging, more than 5600 examinations in more than 8 countries have been evaluated in retrospective or prospective research studies, including a wide variety of patient populations including patients with average, intermediate, and high lifetime risks of breast cancer. , Despite the heterogeneity of the protocols and patient populations, abbreviated breast MR imaging has consistently demonstrated excellent reproducibility with similar accuracy and sensitivity seen across these studies (see Table 1 ). These findings suggest that abbreviated breast MR imaging has the potential to increase breast MR imaging screening use by offering a less expensive, shorter examination that is well-tolerated by patients while preserving the high sensitivity of breast MR imaging for biologically aggressive breast cancer. Various sequences can be included in an abbreviated breast MR imaging protocol; the literature to date has explored the usefulness of which sequences should be included in this examination.
Use of Maximum Intensity Projection Images
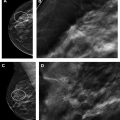
Early studies of abbreviated MR imaging first determined the minimum number of images that needed to be included in a screening protocol. Kuhl and colleagues evaluated the diagnostic accuracy of MIP images alone compared with FAST images and the full diagnostic protocol, with 11 cancers evaluated in 606 screening MR imaging examinations. Although MIP interpretation time was substantially shorter at 2.8 seconds, 10 of 11 cancers were identified. FAST image interpretation was 28 seconds and all 11 cancers were seen, equivalent to the full diagnostic protocol ( Fig. 2 ). The specificity and positive predictive value were also equivalent between FAST images and full diagnostic protocol (94.3% vs 93.9% and 24.4% vs 23.4%, respectively; P = .563 ). Kuhl and colleagues concluded that FAST image interpretation may be preferable to MIP alone. This finding was reinforced by Mango and colleagues, who evaluated 100 biopsy-proven unicentric breast cancers in a 4-reader study using the same sequences as Kuhl and associates. The first postcontrast subtraction image interpretation had a sensitivity of 96% compared with 93% for MIP images. Abbreviated MR imaging acquisition time was 10 to 15 minutes compared with a full protocol of 30 to 40 minutes, with an average interpretation time of 44 seconds ( Fig. 3 ). In this study evaluating only known cancers, missed lesions were more likely to be low-grade invasive cancer or DCIS. Although MIP evaluation can be useful for a quick overview, FAST images should be reviewed carefully to detect subtle lesions.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree