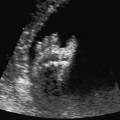
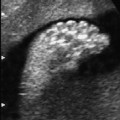
6 Abdomen Definition: Congenital absence of the opening of the anus. Incidence: One in 5000 births. Sex ratio: M : F = 3 : 2. Clinical history/genetics: Sporadic, rarely familial forms with autosomal-recessive inheritance. Embryology: Failure of division of the cloaca into the urogenital sinus and rectum, around 9 weeks after conception. Various lesions are recognized in which the rectum terminates above or below the puborectal sling. The higher the location of anal atresia, the more frequent the associated malformations. The level of atresia also determines whether primary surgical therapy is indicated after birth or whether a colostomy should be performed first, with definitive surgical correction at a later stage. This anomaly is commonly accompanied by esophageal atresia. Teratogens: Alcohol, thalidomide, diabetes mellitus. Associated malformations: These are found in 50%. Skeletal anomalies are associated in 30%, urogenital malformations in 38%, esophageal atresia in 10%, and cardiac anomalies in 5%. Associated syndromes: Over 80 syndromes have been described in which anal atresia is found, including VACTERL association. Various chromosomal anomalies—e.g., partial trisomy 22q and partial monosomy 10q. Ultrasound findings: The anus can be seen as an echogenic spot at the level of the genitals in transverse section. In the case of anal atresia, the echogenic spot is missing. Dilation of the large intestine and calcification of meconium within it may be an additional sign. These findings are first evident at a later gestational age (after 30 weeks). Clinical management: Further sonographic screening, including fetal echocardiography. Karyotyping. Injection of contrast medium into the amniotic cavity followed by radiography of the fetus (amniofetography) have been performed in some cases historically. Procedure after birth: Atretic anus is diagnosed at once at the first examination of the newborn after birth. Oral feeding is then contraindicated. A nasogastric tube should be inserted to relieve the secretions. In male infants, the anal fistula joins the urethra, and in the females the vagina. A blind ending of the rectum is an exception. An anus praeter is often established initially, so that definitive surgical treatment can follow at the age of 6–12 months. Prognosis: This depends on the associated malformations. In the isolated form of anal atresia, 70% of cases show good functional capacity after surgical correction. Self-Help Organizations Title: The Pull-Thru Network Description: A chapter of United Ostomy Association. Support and education of families with children born with anorectal malformations (including cloaca, VATER, cloacal exstrophy, or atretic anus and Hirschsprung’s disease). Maintains a database for personal networking. Quarterly newsletter. Online discussion group. Phone support and literature. Scope: National Number of groups: Two affiliated groups Founded: 1988 Address: 2312 Savoy Street, Hoover, AL 35226–1528, United States Telephone: 205–978–2930 E-mail: pullthru@bellsouth.net Title: TEF/VATER Support Network (Connection) Description: Offers support and encouragement for parents of children with tracheoesophageal fistula, esophageal atresia, and VATER. Aims to bring current information to parents and the medical community. Newsletter, information and referrals, phone support. Scope: International Number of groups: Six groups Founded: 1992 Address: The VATER Connection, 1722 Yucca Lane, Emporia, KS 66801, United States Telephone: 316–342–6954 References Bean WJ, Calonje MA, Aprill CN, Geshner J. Anal atresia: a prenatal ultrasound diagnosis. JCU J Clin Ultrasound 1978; 6: 111–2. Bronshtein M, Zimmer EZ. Early sonographic detection of fetal intestinal obstruction and possible diagnostic pitfalls. Prenat Diagn 1996; 16:203–6. Harris RD, Nyberg DA, Mack LA, Weinberger E. Anorectal atresia: prenatal sonographic diagnosis. AJR AmJ Roentgenol 1987; 149: 395–400. Lam YH, Shek T, Tang MH. Sonographic features of anal atresia at 12 weeks. Ultrasound Obstet Gynecol 2002; 19: 523–4. Lomas FE, Dahlstrom JE, Ford JH. VACTERL with hydrocephalus: family with X-linked VACTERL-H. Am J Med Genet 1998; 76: 74–8. Van Rijn M, Christaens GC, Hagenaars AM, Visser GH. Maternal serum alpha-fetoprotein in fetal anal atresia and other gastro-intestinal obstructions. Prenat Diagn 1998; 18: 914–21. Stoll C, Alembik Y, Roth MP, Dott B. Risk factors in congenital anal atresias. Ann Genet 1997; 40: 197–204. Tongsong T, Wanapirak C, Piyamongkol W, Sudasana I. Prenatal sonographic diagnosis of VATER association. J Clin Ultrasound 1999, 27: 378–84. Definition: Ascites is defined as a collection of fluid within the peritoneal cavity. Clinical history/causes: Fetal hydrops, fetal cardiac insufficiency infections, mediastinal obstruction (pulmonary disease), gastrointestinal obstruction, meconium peritonitis; rarely, perforation in urinary tract obstruction, metabolic and hematological diseases of the fetus, hepatobiliary dysfunction, intra-abdominal tumors. Ultrasound findings: The abdominal scan shows fluid accumulation as an echo-free area in the abdominal cavity. This is usually a clear diagnosis. The greater omentum may often falsely be confused with a cystic lesion in the abdomen. If only a narrow rim of ascites is found, then it is difficult to differentiate from certain artefacts. Clinical management: Further sonographic screening, including fetal echocardiography. It is important to differentiate between isolated fetal ascites and ascites as a part of a generalized fetal hydrops. Are pleural and pericardial effusions present? Can edema of the fetal skin be demonstrated? TORCH serology (prenatal infection?), possibly amniocentesis for further clarification (infection? chromosomal anomaly? cystic fibrosis?). Fig. 6.1 Ascites. Severe isolated fetal ascites at 25 + 6 weeks. The liver, urinary bladder and bowel loops with echoes due to meconium peritonitis are seen floating within it. References Bettelheim D, Pumberger W, Deutinger J, Bernaschek G. Prenatal diagnosis of fetal urinary ascites. Ultrasound Obstet Gynecol 2000; 16: 473–5. Domke N, Luckert G. Fetal ascites in the ultrasound B image. Zentralbl Gynäkol 1984; 106: 15821–6. Gillan JE, Lowden JA, Gaskin K, Cutz E. Congenital ascites as a presenting sign of lysosomal storage disease. J Pediatr 1984; 104: 225–31. Gross BH, Callen PW Filly RA. Ultrasound appearance of fetal greater omentum. J Ultrasound Med 1982; 1: 67–9. Johnson TRJ, Graham D, Sanders RC, Smith N, Simmons MA, Winn K. Ultrasound-directed paracentesis of massive fetal ascites. JCU J Clin Ultrasound 1982; 10: 140–2. Leppert PC, Pahlka BS, Stark RI, Yeh MN. Spontaneous regression of fetal ascites in utero in an adolescent. J Adolesc Health Care 1984; 5: 286–9. Mazeron MC, Cordovi VL, Perol Y. Transient hydrops fetalis associated with intrauterine cytomegalovirus infection: prenatal diagnosis. Obstet Gynecol 1994; 84: 692–4. Meizner I, Carmi R, Mares AJ, Katz M. Spontaneous resolution of isolated fetal ascites associated with extralobar lung sequestration. J Clin Ultrasound 1990; 18: 57–60. Schmider A, Henrich W, Reles A, Vogel M, Dudenhausen JW. Isolated fetal ascites caused by primary lymph-angiectasia: a case report. Am J Obstet Gynecol 2001; 184: 227–8. Straub W, Zarabi M, Mazer J. Fetal ascites associated with Conradi’s disease (chondrodysplasia punctata): report of a case. JCU J Clin Ultrasound 1983; 11: 234–6. Vecchietti G, Borruto F. Ascites of the fetus: intrauterine diagnosis and puncture treatment using ultrasound. Ultraschall Med 1982; 3: 222–4. Zelop C, Benacerraf BR. The causes and natural history of fetal ascites. Prenat Diagn 1994; 14: 941–6. Definition: Complete obliteration of the lumen of the duodenum. Incidence: One in 10 000 births. Clinical history/genetics: Mostly sporadic, rarely familial disposition. Teratogens: Diabetes mellitus, thalidomide. Embryology: The lumen of the intestines is obliterated with epithelium in the 5 weeks after conception: this is a physiological finding. Up until 11 weeks of gestation, recanalization occurs. Duodenal atresia is caused by failure of recanalization. Associated malformations: These are found in 50% of cases. Skeletal anomalies, other gastrointestinal anomalies, especially annular pancreas (20%), cardiac anomalies, and renal malformations. Associated syndromes: Over 15 syndromes with duodenal atresia have been described. Up to a third of the cases have trisomy 21. Ultrasound findings: “Double bubble” sign: the stomach is filled with fluid and next to it, the fluid-filled proximal duodenum can be seen as a second “bubble,” with the pylorus separating the two cavities. The distal bowel is devoid of fluid. Hydramnios frequently coexists, and this is first apparent after 24 weeks. Clinical management: Further sonographic screening, including fetal echocardiography. Karyotyping. Vaginal scan (cervical finding): premature labor? If there is hydramnios with premature contractions and maternal abdominal discomfort, drainage of the hydramnios may be necessary. Procedure after birth: Placement of a nasogastric tube and removal of gastric secretions. The amniotic fluid appears green, due to bile reflux. Aspiration is similar to meconium aspiration. Intubation rather than mask respiration of the infant is preferred to avoid overdistension of the stomach, which facilitates aspiration. Withholding of fluid and nutrients. Early surgical correction with a duodenoduodenal or duodenojejunal anastomosis. Fig. 6.3 Duodenal atresia. Same findings as above, in longitudinal section. Prognosis: This depends on coexisting malformations and the maturity of the infant (premature labor due to hydramnios). Mortality can be as high as 36%. Surgical repair of isolated duodenal atresia is successful in almost all cases, with an overall survival rate of 95%. References Collier D. Antenatal diagnosis of duodenal atresia by ultrasound: a case report. Radiography 1982; 48: 102–3. Dundas KC, Walker J, Laing IA. Oesophageal and duodenal atresia suspected at the 12 week booking scan. BJOG Br J Obstet Gynecol 2001; 108: 225–6. Fletman D, McQuown D, Kanchanapoom V, Gyepes MT. “Apple peel” atresia of the small bowel: prenatal diagnosis of the obstruction by ultrasound. Pediatr Radiol 1980; 9: 118–9. Grosfeld JL, Rescorla FJ. Duodenal atresia and stenosis:reassessment of treatment and outcome based on antenatal diagnosis, pathologic variance, and long-term follow-up. World J Surg 1993; 17: 301–9. Hösli KI, Tercanli S, Nars PW, Holzgreve W. Combined esophageal atresia and duodenal stenosis in polyhydramnios: ante-, peri- and postpartum management. Z Geburtshilfe Neonatol 1996; 200: 161–5. Lawrence MJ, Ford WD, Furness ME, Hayward T, Wilson T. Congenital duodenal obstruction: early antenatal ultrasound diagnosis. Pediatr Surg Int 2000; 16: 342–5. Nelson LH, Clark CE, Fishburne JI, Urban RB, Penry MF. Value of serial sonography in the in utero detection of duodenal atresia. Obstet Gynecol 1982; 59: 657–60. Ranzini AC, Guzman ER, Ananth CV, Day-Salvatore D, Fisher AJ, Vintzileos AM. Sonographic identification of fetuses with Down syndrome in the third trimester: a matched control study. Obstet Gynecol 1999; 93: 702–6. Salihu HM, Boos R, Schmidt W. Antenatally detectable markers for the diagnosis of autosomally trisomic fetuses in at-risk pregnancies. Am J Perinatol 1997; 14: 257–61. Stoll C, Alembik Y, Dott B, Roth MP. Evaluation of prenatal diagnosis of congenital gastro-intestinal atresias. Eur J Epidemiol 1996; 12: 611–6. Tsukerman GL, Krapiva GA, Kirillova IA. First-trimester diagnosis of duodenal stenosis associated with oesophageal atresia. Prenat Diagn 1993; 13: 371–6. Definition: Congenital atresia or stenosis of the small or large bowel. Incidence: Small-bowel atresia and stenosis occur in one in 3000–5000 births (jejunum 50%, ileum 43%, multiple stenosis 7%). Large-bowel atresia and stenosis one in 20 000. Clinical history/genetics: Mostly sporadic. Autosomal-recessive syndromes have been described in association with intestinal atresia and stenosis. Cystic fibrosis is found in 25% of cases of jejunal and ileum atresia. Teratogen: Thalidomide, cocaine; application of methylene blue (e.g., amniocentesis in twin pregnancy). Embryology: Most cases are attributed to a vascular accident (hypotension, vessel anomaly, volvulus) causing local ischemia. Three types of stenosis are described: 1. Bowel continuity is disturbed by a membrane consisting of mucous and submucous parts. The tunica muscularis is not involved.
Anal Atresia
Ascites

Duodenal Atresia


Intestinal Atresia and Stenosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree