Anatomy, embryology, pathophysiology
- ◼
There are five distinct densities in plain radiography, four of which are natural: gas (black), fat (dark gray), soft tissue (medium gray), calcifications (white), and metal (intense white).
- ◼
Dedicated assessment of each density is essential in any search pattern.
Techniques
- ◼
The standard abdominal radiograph is obtained in a supine projection, with x-rays passing from anteroposterior (AP). Field of view should span the inferior ribs to the inferior pubic rami, and include both lateral abdominal walls.
- ◼
Additional projections can be obtained to assess for free air or air-fluid levels. These include upright positioning (erect) or with the patient lying on his or her side (lateral decubitus). The erect view is typically preferred for ease of use and must include the diaphragm even at the expense of the pelvis. A lateral decubitus view can be alternatively performed in patients unable to tolerate upright imaging.
Specific disease processes
Intraluminal gas
There is wide variation in the appearance of a normal bowel gas pattern.
- ◼
Gas in the left upper quadrant (stomach) can produce a gastric bubble on erect imaging. If distended with air or ingested contrast, the normal gastric rugae can be a distinguishing feature.
- ◼
The small bowel is comprised of the duodenum, jejunum, and ileum. It is identified on radiography by the presence of circumferential folds called valvulae conniventes (or plicae circulares) that traverse the entire width of the small bowel. The jejunum begins at the ligament of Treitz and primarily resides in the left upper quadrant. The increased folds of the jejunum give it a feathery pattern. In contrast, the ileum is usually larger in caliber and contains fewer folds, producing a more featureless mucosal pattern. In general, the small bowel should be less than 3 cm in diameter.
- ◼
The large bowel (or colon) extends from the ileocecal valve to the anus, and comprises the cecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum. The large bowel is distinguished by haustra, which are large folds that only cross portions of the bowel wall. Large bowel contains feculent material that often gives a mottled appearance, representing a mixture of gas/liquid/solid material. The cecum can be normal at up to 9 cm in diameter, whereas the remainder of the large bowel can distend normally up to 6 cm.
Extraluminal gas
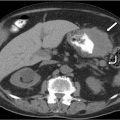
Extraluminal gas outside of the bowel lumen can range from atypical to grossly pathological ( Fig. 1.1 ).
- ◼
Gas within the peritoneal cavity is called pneumoperitoneum. This is best identified on erect imaging, which will show free air under the diaphragm, particularly on the right ( Fig. 1.2 ). Caution must be exercised to identify the normal left upper quadrant stomach bubble when evaluating for free air on the left. On decubitus imaging, free air will appear clearly outside the contours of the bowel lumen, rising to the antidependent portion of the radiograph.

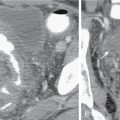
Fig. 1.2
Upright KUB demonstrates free air under the diaphragm, the so called “continuous diaphragm sign.”
- ◼
Small volumes of postoperative pneumoperitoneum can be an expected finding within 7 to 10 days after surgery. If there has been no history of recent intervention, or if the volume of pneumoperitoneum is larger than expected, there should be a concern for pathological hollow viscus perforation.
- ◼
In the absence of upright or decubitus projections, large volume pneumoperitoneum can be identified by a variety of signs, including Rigler’s sign, football sign and so on. ( Fig. 1.3 ).

Fig. 1.3
Portable anteroposterior KUB demonstrates pneumoperitoneum with Rigler’s sign. Note the conspicuity of the bowel walls because of air outlining both sides.
- ◼
Gas in the bowel wall (pneumatosis) can occur in a variety of benign or pathological processes. Correlation with history is essential as pneumatosis can be iatrogenic (e.g., related to recent G-tube placement), pathological (related to bowel ischemia), medication-related (i.e., chemotherapy) or idiopathic.
- ◼
Air can also be seen overlying the liver. Gas within the bile ducts (pneumobilia) can be seen in the presence of a sphincterotomy, biliary stent, biliary bypass, or biliary fistula. Pneumobilia should overlie the central liver. Air that extends to the periphery of the liver may reflect portal venous gas, which is always pathological. Gas in the portal vein is typically a result of bowel ischemia and may be an ominous sign.

Calcifications
Calcium deposits in a wide variety of normal and abnormal structures.
- ◼
Benign aortic calcifications are common and can help visualize the borders of the aorta and major branches. Large aortic and branch vessel aneurysms can be identified by the demarcation of their associated wall calcifications.
- ◼
Pancreatic calcifications overlying the mid-abdomen can be seen in chronic pancreatitis.
- ◼
Calcified renal or bladder calculi can be seen overlying the expected renal fossa and bladder. These should be distinguished from pelvic phleboliths, which are extremely common, especially in elderly adults. Phleboliths tend to be rounder and have a radiolucent center, as well as a more lateral position in the pelvis compared with urolithiasis.
- ◼
Densely calcified gallstones or a calcified (porcelain) gallbladder can often be seen in the right upper quadrant.
- ◼
Uterine fibroids can often become calcified. Ovarian dermoid cysts are also an uncommon cause of pelvic calcifications.
- ◼
Other unusual causes of calcifications include calcified lymphadenopathy, remote fat necrosis and “dropped gallstones.”
Soft tissues and bone
The outlines of the major abdominal organs can often be distinguished by their surrounding fat planes. Patients with cachexia or extreme weight loss may lose these fat planes, making the identification of normal abdominal organs difficult. Similarly, disruption of the normal fat planes can be a secondary clue for ascites or hemoperitoneum.
- ◼
The liver and gallbladder are located in the right upper quadrant. A Riedel lobe is a normal anatomic variant where the right liver projects inferiorly to the level of the pelvis.
- ◼
Splenomegaly can be noted with mass effect upon the normal bowel gas in the left hemiabdomen.
- ◼
Both kidneys can often be visualized around the T12-L2 vertebral body levels. The psoas muscle shadows are just medial to each kidney and mark the course of both ureters.
- ◼
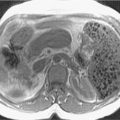
Large abdominal soft tissue masses can produce mass effect on the adjacent structures, particularly the bowel gas.
- ◼
The imaged osseous structures include the lower spine, pelvis, and proximal hips and femurs. A wide variety of pathology includes fractures, sclerotic and lytic metastases; inflammatory disease and degenerative changes can be seen.
Foreign bodies
Foreign bodies should be evaluated for appropriateness and positioning whenever possible.
- ◼
Iatrogenic lines and tubes, such as nasogastric or percutaneous gastrostomy tubes, biliary tubes, nephrostomy tubes, ureteral stents, peritoneal drainage catheters and peritoneal dialysis catheters ( Fig. 1.4 ).