Chapter Outline
Mechanisms of Injury in Abdominal Trauma
Diagnostic Techniques in Patients with Abdominal Trauma
Computed Tomography Use in Abdominal Trauma
Computed Tomography Imaging Techniques and Interpretation
Approach to Computed Tomography Interpretation
Computed Tomography Findings in Abdominal Injury
Computed Tomography and Bowel Injury
Computed Tomography Findings in Bowel and Mesenteric Injury
Trauma is the leading cause of death in Americans younger than 45 years and the fifth leading overall cause in the United States. Preliminary data approximate that more than 122,000 people died of traumatic injury in 2011. Trauma has a significant economic burden on U.S. health care, with more than 45 million emergency department visits every year and approximately $80 billion spent in direct medical costs. It is also the leading cause of disability and exceeds any other disease in productive years lost. In the year 2000, productivity losses due to trauma cost the United States $326 billion.
Appropriate prompt evaluation of trauma patients is essential to avoid serious morbidity and mortality. Although the physical examination is still vital in the initial assessment of these patients, some studies have shown sensitivity in the range of only 55% to 65% in the setting of blunt abdominal trauma. Furthermore, patients who show no obvious signs of trauma or physical examination findings (such as a seat belt sign, abdominal tenderness, or guarding) may still have significant internal organ injury. Therefore, imaging has come to play a critically important role in trauma diagnosis and management.
In this chapter, we describe the mechanisms of injury in abdominal trauma as well as the role of imaging modalities—with a focus on computed tomography (CT)—in the evaluation of the trauma patient. We also review CT imaging techniques and the diagnostic criteria used for interpretation in abdominal trauma, with an emphasis on the role of abdominal CT in bowel injury.
Mechanisms of Injury in Abdominal Trauma
Abdominal injury can be divided into blunt and penetrating subtypes. Blunt trauma is the cause of more than 80% of abdominal injuries, whereas penetrating injuries account for approximately 20%. Penetrating injuries include stab and gunshot wounds, with stab wounds being encountered approximately three times more often than gunshot wounds. Penetrating trauma can have a more straightforward evaluation compared with blunt injury in that the point of wound entry is usually evident, and in the case of gunshot wounds, the exit wound can also be identified. However, the extent of injury with blunt trauma is less conspicuous on physical examination and is thus associated with higher morbidity and mortality.
Most blunt injuries occur after a motor vehicle collision, followed by a pedestrian versus vehicle collision and direct blows to the abdomen by falls, assaults, or sports injuries. Three mechanisms are often used to describe blunt trauma. These are deceleration injuries, crush injuries, and external compression. Rapid deceleration creates significant shearing forces between fixed and mobile parts of organs that can result in lacerations at these areas or at points of attachment to the peritoneum. These forces can also lead to vascular tears or cause stretch injuries to arteries, resulting in infarction of susceptible organs. External objects such as the seat belt or steering wheel can lead to crush injury of the organs between the abdominal wall anteriorly and the thoracic ribs or vertebral column posteriorly. Finally, a sudden increase in intra-abdominal pressure by external compression can lead to perforation of hollow viscera.
Oftentimes, more than one mechanism occurs during the traumatic incident with simultaneous injury to multiple organs. For instance, an unrestrained driver in a motor vehicle accident who is ejected from the vehicle could initially strike the windshield, producing the first set of injuries, and then could strike the ground outside the vehicle, producing a second set of injuries. If the patient is still moving rapidly, a third or fourth set of injuries may occur until the patient eventually comes to a stop. Injuries may be clustered in one portion of the body, but multiple sites of injury may exist in the same patient. Thus, in assessing patients with history of trauma, it is helpful to know details of the type of trauma as this can be useful in determining specific patterns of injured organs. In addition, the mechanism of injury has been found to be an independent predictor for mortality and long-term functional impairment.
The spleen is the most commonly injured intra-abdominal organ and may be the only affected organ in up to 60% of cases. Following the spleen, in order of decreasing frequency, the other commonly injured organs are the liver, kidneys, small bowel or mesentery, bladder, colon or rectum, diaphragm, pancreas, and major vessels.
Diagnostic Techniques in Patients with Abdominal Trauma
The diagnostic approach to trauma patients varies according to their hemodynamic status. Patients who remain hemodynamically unstable despite appropriate resuscitation efforts are usually taken to the operating room for emergent laparotomy because of high suspicion of ongoing hemorrhage. Diagnostic techniques for abdominal trauma include the focused assessment with sonography for trauma (FAST) and diagnostic peritoneal lavage. In short, FAST is used to evaluate for free intraperitoneal fluid and is usually performed before exploratory laparotomy. It is a rapid, noninvasive test that can be performed at the bedside and has been shown to have up to 90% specificity for blood products in the abdomen and pelvis. However, it is an operator-dependent examination that does not focus on direct signs of organ trauma. It also has a low sensitivity (29%-35%) for organ injury in the absence of hemoperitoneum. Because intra-abdominal injury cannot be ruled out with normal findings on FAST scan, further diagnostic testing, such as diagnostic peritoneal lavage or CT, is often necessary.
Diagnostic peritoneal lavage is used to evaluate for intra-abdominal hemorrhage and hollow organ injury. Its use has markedly decreased because of advances in imaging technology and increased nonoperative management after trauma. The principle of this technique is to infuse saline into the peritoneum to mix with possible blood and then to recover the fluid for analysis. Diagnostic peritoneal lavage has high sensitivity in the detection of peritoneal bleeding, and some trauma surgeons appreciate its capacity of providing them prompt and easy-to-interpret information in settings in which radiologists are not readily available to interpret films. However, its disadvantages include lack of specificity for the source of bleeding and that it is an invasive procedure with associated risks and morbidity.
Computed Tomography Use in Abdominal Trauma
The speed and accuracy of CT as well as its widespread availability in emergency departments and trauma centers have led this imaging modality to play a principal role in the triage and diagnosis of trauma patients. Although the use of CT in abdominal trauma dates to the 1980s, the advent of helical scanning and multidetector helical computed tomography (MDCT) has allowed it to be more widely used with reduced scan times and improved image quality.
In the past, trauma patients were initially evaluated with conventional chest, cervical spine, and pelvic radiographs. CT scans were obtained only for hemodynamically stable patients with blunt abdominal trauma, in those with no evidence of penetrating injury, or in those who presented obtunded. Today, CT is more frequently used in patients with some degree of clinical instability, provided they respond to initial resuscitation and are stable enough to undergo CT. In fact, a study published in 2009 found that of patients who underwent whole-body CT, one of every five had been in shock at the scene of the trauma and one of six at the time of admission. CT is now also routinely used in patients with chest injuries or penetrating wounds.
When it comes to clinical decision making, CT scanning has proved to be superior to other methods in the diagnosis of injuries that require surgical intervention. In a study conducted by Deunk and coworkers, researchers found that MDCT findings after trauma often result in a change in treatment decisions. Moreover, increased CT use after trauma has led to a shift to nonoperative management and decreased morbidity and in-hospital mortality. A large number of injuries involving the liver, spleen, and kidneys are now managed conservatively if patients are hemodynamically stable.
Computed Tomography Imaging Techniques and Interpretation
Trauma CT protocols should attempt to optimize images to help radiologists detect injuries while minimizing risks to the patient. To achieve this goal, it is important to consider various aspects of image acquisition and analysis. These include the use of contrast material, different phases of acquisition with their varying degrees of contrast enhancement, radiation dose, and image processing.
Contrast Material
The intravenous use of contrast material improves the sensitivity and specificity of CT for detection of injury. The American College of Radiology developed the Appropriateness Criteria, which are evidence-based guidelines meant to aid in the selection of imaging and routes of administration of contrast material in different emergency scenarios. The guidelines state that the intravenous use of contrast material is critical to identify bowel, visceral, or vascular injury in the setting of blunt abdominal trauma. In addition, they recommend against the use of oral contrast material in the setting of blunt abdominal injury, probably because of lack of additional diagnostic value as well as potential delay in obtaining the CT images owing to wait time for enteric contrast material to progress.
One of the more controversial issues surrounding the intravenous use of contrast material is the risk of acute kidney injury, especially in the elderly, those with established renal insufficiency, and patients with chronic diseases, such as diabetes mellitus, congestive heart failure, and hypertension. This is especially worrisome in the setting of trauma, when oftentimes one cannot obtain a thorough history and testing for renal function might delay possible treatment.
Some centers have recently been looking at point-of-care (POC) creatinine testing in patients presenting for imaging with nonspecific history that could be concerning for kidney disease. A study by Lee-Lewandrowski and colleagues looked at POC creatinine testing and its impact on clinical operations in the radiology department of a large academic medical center. This group found that 5.3% of patients (441 per month) who presented for scans did not have a recent creatinine level or estimated glomerular filtration rate; 26% of these were determined to be abnormal. They also found good agreement between POC and central laboratory plasma creatinine testing; however, the POC creatinine testing was approximately 47% more expensive than central laboratory plasma creatinine testing. However, because of the increased timeliness and improved quality of scans with intravenous contrast material, the authors suggested that POC creatinine testing improves clinical operations and is likely to be cost-effective. A study of POC creatinine testing in the emergency department also showed good correlation between POC and serum testing, leading the authors to conclude that because of its ease of use and rapid turnaround time, it could be of substantial benefit in the emergent setting.
Multiphasic Imaging
Because of increased image acquisition speed, it is possible to achieve multiphasic imaging with a single bolus of contrast material. However, there is no current consensus on the optimal number of phases needed for a trauma protocol as peak contrast enhancement varies between organs and there are advantages to each of the phases. Some researchers believe that the portal venous phase, which occurs 65 to 80 seconds after initiation of administration of the contrast material, is a good compromise in the diagnosis of parenchymal injury. In a study of the role of multiphasic imaging in pancreatic injury detection, for instance, researchers found that the portal venous phase was the most accurate to determine signs suggestive of ductal injuries. Results of a study on splenic trauma by Boscak and associates showed that the portal venous phase was more sensitive than the arterial phase in the diagnosis of parenchymal injury and active hemorrhage, yet the arterial phase was more sensitive for pseudoaneurysm detection. The authors suggested that dual phase imaging offers optimal overall performance.
Multiphasic imaging is also beneficial in trying to further characterize vascular injuries. Acquiring images at different points in time helps differentiate between contained injury and active vascular hemorrhage as well as distinguish arterial from venous sources. By using delayed imaging, one can theoretically characterize the rate of bleed by looking for enlarged areas of extravasation of contrast material as well as evaluate the collecting system of the kidneys.
Radiation Dose
With regard to radiation dose, as with all imaging, a risk-benefit analysis needs to be performed for each patient to determine if CT is appropriate. Specifically, the risks of radiation and intravenous administration of contrast material must be weighed against the benefits from diagnosis of traumatic injuries. In light of the fact that CT is superior to clinical evaluation and modalities such as diagnostic peritoneal lavage for diagnosis of clinically significant abdominal injuries, CT is a mainstay in the imaging of acute traumatic injury. It is critical to adhere to the concept of ALARA (as low as reasonably achievable) in performing CT; that is, image quality should be maximized but not at the expense of increased radiation dose to the patient. As such, there are multiple dose reduction tools available on current CT scanner platforms, including automatic tube current modulation, which allows the tube current to automatically change with the region of the body being imaged, thereby lowering radiation dose. In addition, whereas most CT is reconstructed with conventional filtered back projection, new research is focused on a host of new iterative reconstruction algorithms designed to reduce dose while maintaining image quality. Willemink and associates recently showed that although the mean time required for CT image reconstruction for whole-body trauma CT is statistically significantly higher with iterative reconstruction as opposed to filtered back projection, this difference is on the order of 45 seconds, likely making this a clinically insignificant delay in the trauma setting. This study was limited in that it was performed with one CT vendor’s software only; additional studies with the other major vendor’s iterative reconstruction products are likely needed to assess whether this holds true for other iterative reconstruction algorithms.
Image Processing
Current multidetector CT platforms have the ability to acquire data at submillimeter section thickness with isotropic data sets. Interpretation of these submillimeter-thick data sets can be cumbersome, and most centers will reconstruct these images at 2.5- or 5.0-mm section thickness to facilitate image interpretation.
In addition, reconstruction of axial data sets in the coronal and sagittal planes can often be performed by the CT technologist at the console and sent to a picture and archiving communication system for interpretation by the radiologist in conjunction with the axial data sets. Coronal and sagittal reconstructions have the ability to help confirm diagnoses made on axial images as well as to aid in diagnosis of injuries of other structures, such as the bladder, diaphragm, and spine ( Fig. 126-1 ).

Approach to Computed Tomography Interpretation
The mechanisms of traumatic injuries are often complex and can lead to multiorgan injury. As such, a consistent and repeatable search pattern can help minimize missed injuries. The use of a rigorous routine in the interpretation of trauma patient CT studies significantly diminishes the number of missed traumatic lesions, especially in the setting of multiple injuries. As with any CT interpretation, the specific search pattern used is less important than simply having and following a comprehensive search pattern in each case.
Computed Tomography Findings in Abdominal Injury
Liver and Spleen
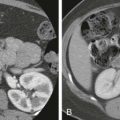
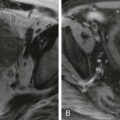
Currently, most splenic and liver injuries are managed conservatively in the hemodynamically stable patient. The major types of blunt hepatic and splenic trauma include subcapsular and intraparenchymal hematomas ( Fig. 126-2 ), lacerations ( Fig. 126-3 ), active hemorrhage, and other vascular injuries. Of note, vascular injury can be subtle, and its only sign may be end-organ damage. The American Association for the Surgery of Trauma (AAST) has devised injury grading scales for both liver and splenic injuries ( Tables 126-1 and 126-2 ).


| Grade * | Lesion | Injury Description |
|---|---|---|
| I | Hematoma | Subcapsular, <10% surface area |
| Laceration | Capsular tear, <1 cm parenchymal depth | |
| II | Hematoma | Subcapsular, 10% to 50% surface area |
| Intraparenchymal, <10 cm in diameter | ||
| Laceration | Capsular tear, active bleeding 1-3 cm parenchymal depth, <10 cm in length | |
| III | Hematoma | Subcapsular, >50% surface area or ruptured with active bleeding Intraparenchymal hematoma >10 cm or expanding |
| Laceration | >3 cm parenchymal depth | |
| IV | Laceration | Parenchymal disruption involving 25% to 75% of hepatic lobe or 1-3 Couinaud segments within a single lobe |
| V | Laceration | Parenchymal disruption involving >75% of hepatic lobe or >3 Couinaud segments within a single lobe |
| Vascular | Juxtahepatic venous injuries (i.e., retrohepatic vena cava and/or central major hepatic veins) | |
| VI | Vascular | Hepatic avulsion |
* Advance one grade (up to grade III) for multiple injuries.
| Grade * | Lesion | Injury Description |
|---|---|---|
| I | Hematoma | Subcapsular, <10% surface area |
| Laceration | Capsular tear, <1 cm parenchymal depth | |
| II | Hematoma | Subcapsular, 10% to 50% surface area |
| Intraparenchymal, <5 cm in diameter | ||
| Laceration | Capsular tear, active bleeding 1-3 cm parenchymal depth, does not involve trabecular vessels | |
| III | Hematoma | Subcapsular, >50% surface area or expanding Ruptured subcapsular or intraparenchymal hematoma Intraparenchymal hematoma >5 cm or expanding |
| Laceration | >3 cm parenchymal depth or involves trabecular vessels | |
| IV | Laceration | Involves segmental or hilar vessels, producing major devascularization (>25% of spleen) |
| V | Laceration | Completely shattered spleen |
| Vascular | Hilar vascular injury that devascularized the spleen |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree