Multidetector CT (MDCT) is the imaging method of choice for the diagnosis of intra-abdominal injury following blunt abdominal trauma. Treatment is directed by characterization of the precise nature of the injury, or by the reliable demonstration of the absence of significant injury. CT is particularly valuable when physical examination of the abdomen is equivocal or unreliable, such as with head trauma or impairment of consciousness caused by drugs or alcohol. CT has the advantage of evaluating the entire abdomen and pelvis in a single comprehensive study. The sensitivity of CT for detecting intra-abdominal injury exceeds 90%.
Patients who have had significant blunt abdominal trauma and who are hemodynamically stable are candidates for trauma CT of the abdomen. Patients who are hemodynamically unstable, who have signs of peritonitis, or who have had penetrating abdominal trauma are candidates for immediate exploratory surgery, which should not be delayed by CT. On the other hand, patients with a history of blunt abdominal trauma who do not have physical examination evidence of traumatic injury to the abdomen receive little benefit from trauma CT.
At many institutions limited ultrasound examination is used to perform a rapid screening of the abdomen and pelvis to detect the presence of free intraperitoneal fluid (focused abdominal sonography for trauma [FAST] scan). If fluid is present, trauma CT of the abdomen and pelvis is performed. If fluid is absent and clinical assessment is low risk, trauma CT may be deferred, although not all significant intra-abdominal injuries are associated with hemoperitoneum. The sensitivity of ultrasound imaging for free intraperitoneal fluid is 63%. It is limited primarily by lack of bladder filling impairing visualization of fluid in the cul-de-sac. Routine filling of the bladder with 200 to 300 mL of sterile saline increases sensitivity to 84%. In females of reproductive age and in children, free fluid limited to the cul-de-sac is most likely physiologic.
Scan Technique
Intravenous contrast agent administration is the most critical component in the performance of trauma CT of the abdomen. Solid organ enhancement confirms the presence of blood flow and provides the optimal detection of lacerations and hematomas, which may be isodense in unenhanced organs. All trauma CT scans must include both the abdomen and the pelvis. Extensive hemorrhage may settle dependently in the pelvis and be barely detectable on scans confined to the abdomen. All CT images should be viewed with lung windows to detect pneumothorax and pneumoperitoneum, with bone windows to detect bone injuries, and with routine soft-tissue windows to reveal organ injury.
The use of oral contrast agent before trauma CT scans remains controversial, with most institutions now scanning without oral contrast agent in the setting of trauma. Extended patient preparation with oral contrast agent may inappropriately delay CT scanning. Patients may vomit or aspirate oral contrast agent. Oral contrast agent may interfere with the performance of angiography, if needed in the treatment of active hemorrhage. Oral contrast agent is often poorly distributed through the bowel because of ileus induced by trauma. At our institution we routinely scan acute trauma patients without oral contrast agent. A number of studies, including our own, have documented no significant change in the accuracy of trauma CT without the use of oral contrast agent. Water may serve as an effective agent to distend the stomach and proximal part of the bowel without the disadvantages of positive contrast agents. When possible and without causing delay in obtaining the CT scan, 400 to 700 mL of water may be given orally or via a nasogastric tube.
For trauma CT scans, helical MDCT is performed with a 70-second delay (portal venous phase scan) following intravenous injection of 150 mL of iodinated contrast agent by a power injector at 3.5 mL per second. Images are viewed at 2.5- to 5.0-mm slice thickness. Delayed scans through the kidneys at 5 to 10 minutes are performed to evaluate patients for rupture of the collecting system if the initial scan shows perirenal fluid or other signs of renal injury. The entire abdomen and pelvis are scanned from the dome of the diaphragm through the ischial tuberosities. If the chest is also being evaluated by panscan CT, imaging is continued throughout the abdomen and pelvis without overlap. In select cases an arterial phase scan at 25 to 30 seconds after intravenous contrast agent injection may be added to assess patients for active hemorrhage. Indications for the arterial phase scan include severe mechanism of injury, clinical suspicion of active bleeding, and known displaced fractures of the pelvis.
CT cystography should be performed if bladder injury is suspected because of gross hematuria, significant trauma to the pelvis, the presence of pelvic fractures, or stranding or fluid around the bladder. The bladder must be actively distended to a minimum of 250 mL to demonstrate or to exclude bladder rupture. Passive filling of the bladder by intravenous contrast agent is not sufficient to exclude bladder injury. CT cystography is performed by instillation of 250 to 300 mL of 3% to 5% iodinated contrast agent into the bladder via a Foley catheter. Scans are obtained through the pelvis before and after contrast agent instillation with images reconstructed at 3- to 5-mm thickness. Post–bladder drainage scans are not necessary.
Trauma CT and the Pregnant Patient
In the pregnant patient radiation exposure is an appropriate concern. However, trauma is a leading cause of nonobstetric maternal death and fetal loss. Pregnancy itself increases the risk of intra-abdominal traumatic injury. Maternal death nearly always results in fetal death. Although each case should be evaluated individually, in the setting of major abdominal trauma to the pregnant patient the risk of a missed or delayed diagnosis of major traumatic injury far outweighs the low risk of radiation exposure. Care should be taken to ensure that the lowest possible radiation dose be used to obtain a diagnostic trauma CT scan. Ultrasonography is used to determine the well-being of the fetus.
CT Findings of Traumatic Injury
CT findings of traumatic injury within the abdomen or pelvis include the following:
- •
Hemoperitoneum. Blood within the peritoneal cavity is a highly reliable sign of intra-abdominal injury ( Fig. 10.1 ). Fresh unclotted blood measures 30 to 45 Hounsfield units (HU) compared with 0 to 15 HU of ascites or serum. Separation of clotted blood and serum may result in visible fluid layers ( hematocrit effect ). Fresh blood flows from the area of injury to dependent peritoneal recesses in the abdomen and pelvis. Small volumes of low-attenuation fluid (10–15 HU) may be considered a normal finding in children, adult males, and females during their menstrual cycle. Rarely attenuation of liquid blood may be less than 20 HU if the patient has anemia or preexisting ascites.

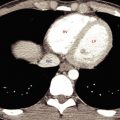
FIG. 10.1
Hemoperitoneum.
(A) Contrast-enhanced CT through the upper abdomen shows hemoperitoneum (H) enveloping the liver (L) and spleen (S) . Multiple lacerations of the spleen are evident as low-attenuation clefts (yellow arrowheads) through the enhanced splenic parenchyma. A higher-attenuation blood clot (C) is seen adjacent to the spleen. Note the difference in attenuation between clot and liquid blood (red arrow) . This patient received an oral contrast agent, which distends the stomach (St) . (B) CT image of the pelvis showing blood (H) settling in the peritoneal recesses of the pelvis surrounding the bladder (B) and uterus (U) .
- •
Sentinel clot. A focal collection of clotted blood (45–70 HU) is an accurate marker of injury to the adjacent organ ( Figs. 10.1A and 10.2 ). Occasionally the sentinel clot is the only positive finding of specific organ injury. The higher-density clot stands out in relief compared with lower-density unclotted blood or serum.

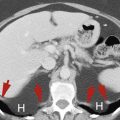
FIG. 10.2
Sentinel clot.
A high-attenuation blood clot (yellow arrowheads) serves as a marker of a poorly visible laceration (red arrow) in the spleen (S) . Lower-attenuation blood (H) is seen in the recesses of the peritoneal cavity around the spleen. A rib fracture (curved arrow) is also present.
- •
Active bleeding. Active hemorrhage may be detected by scanning during the arterial phase of dynamic intravenous contrast agent administration. Active extravasation is seen as hyperdense foci within areas of lower-density liquid blood ( Fig. 10.3 ). The attenuation of active hemorrhage ranges from 85 to 370 HU and is usually within 20 HU of the attenuation of nearby arteries such as the aorta. On delayed images the focal contrast agent collection fades into the surrounding hematoma. This finding is a sign of life-threatening hemorrhage and often necessitates immediate angiographic or surgical therapy.

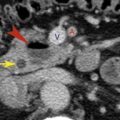
FIG. 10.3
Active hemorrhage.
Contrast-enhanced trauma CT of the liver during the arterial phase shows a focus of active hemorrhage (arrow) seen as an amorphous extravascular collection of contrast agent within a low-attenuation hepatic hematoma. Compare the attenuation of the contrast agent collection with that of the enhanced aorta (A) . Extensive hemoperitoneum (H) is evident.
- •
Free air in the peritoneal cavity is a sign of transmural bowel laceration ( Fig. 10.4 ). Unfortunately this sign is neither sensitive nor specific. Extraluminal air is found in only 32% to 55% of cases of bowel laceration. Free air may also result from diagnostic peritoneal lavage, barotrauma, or mechanical ventilation. Additional findings of bowel injury must be present before this finding is definitively ascribed to bowel perforation. Pneumoperitoneum appears as very low attenuation extraluminal collections of gas in the anterior abdomen in the supine patient. Free air is best detected on lung windows.

FIG. 10.4
Pneumoperitoneum.
CT image of the abdomen shown with lung windows demonstrating an extraluminal collection of air (red arrow) anterior to the liver. This patient had a traumatic laceration of the jejunum. Serial images are inspected to ensure that no bowel containing gas in the lumen is in this area. Compare this with gas within the bowel (B) limited by a thin bowel wall (yellow arrow) .
- •
Free contrast agent in the peritoneal cavity may occur with extravasation of oral contrast agent through a bowel perforation or from leakage of contrast-opacified urine from the urinary tract ( Fig. 10.5 ). Extraluminal oral contrast agent is found in only 14% of bowel transections. Additional findings such as bowel wall thickening and blood in the mesentery confirm bowel injury as the source of extraluminal contrast agent. Extravasated contrast agent–containing urine should be seen on delayed images after the renal collecting systems, ureter, and bladder fill with contrast agent.

FIG. 10.5
Free intraperitoneal contrast agent.
Image through the upper abdomen revealing high-density contrast agent in the peritoneal recesses (arrowheads) . This patient had an intraperitoneal rupture of the bladder. Contrast agent excreted in the urine was extravasated through the hole in the bladder into the peritoneal cavity.
- •
Subcapsular hematomas appear as crescent-shaped collections that flatten and indent the organ parenchyma ( Fig. 10.6 ). Attenuation is lower than that of contrast-enhanced organ parenchyma. The outer border of the collection is sharply defined by the capsule of the involved organ. The inner margin compresses adjacent parenchyma.

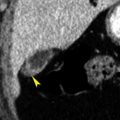
FIG. 10.6
Subcapsular hematoma.
The contour (arrowheads) of the right kidney (RK) is compressed and distorted by a hematoma (H) confined within the restricted space bounded by the renal capsule. This finding is indicative of subcapsular location of the hematoma.
- •
Intraparenchymal hematomas are seen as irregularly shaped rounded low-attenuation collections within contrast-enhanced parenchyma ( Fig. 10.7 ). Small intraparenchymal hematomas are commonly called contusions. Flow defects during contrast enhancement of the normal spleen should not be mistaken for intrasplenic hematomas (see Fig. 14.3 ).

FIG. 10.7
Intraparenchymal hematomas.
Multiple intraparenchymal hematomas (arrows) are seen as low-attenuation defects within the contrast-enhanced splenic parenchyma.
- •
Lacerations are jagged linear, often branching, defects in organ tissue that are defined by lower-density blood within the laceration ( Fig. 10.8 ). Most lacerations extend through the organ capsule and are associated with hemoperitoneum.

FIG. 10.8
Liver laceration.
Traumatic laceration (arrows) of the liver is seen as a jagged low-attenuation defect with the enhanced liver parenchyma. Blood and bile within the laceration are responsible for the low attenuation of the laceration. Contrast enhancement of the liver accentuates the lesion.
- •
Shattered organs are disrupted by multiple lacerations ( Fig. 10.9 ). Shattered organs are frequently associated with multiple infarcted segments of parenchyma. Portions of enhanced and nonenhanced organ parenchyma may be widely dispersed by hemorrhage.

FIG. 10.9
Shattered spleen.
Multiple lacerations (arrows) are seen as jagged defects in the parenchyma of the spleen (S) .
- •
Absence of parenchymal enhancement is an indication of loss of vascular supply ( Fig. 10.10 ). The supplying artery may be lacerated or thrombosed. The entire organ, or only a portion of the organ, may be affected.