Anatomy, embryology, pathophysiology
- ◼
Injuries depend upon patient composition, blunt versus penetrating injury, mechanism of injury, and strength of forces.
- ◼
Blunt trauma etiologies: motor vehicle crash, falls, assault, and sports resulting in deceleration/shear forces, crushing forces, and increased intraabdominal pressure.
- ◼
Major cause of preventable death is intraabdominal hemorrhage.
Techniques
Radiography
- ◼
Rapid and portable, facilitating use in the critically ill patient for detection of:
- ◼
Intraperitoneal free air (although challenging on supine radiograph).
- ◼
Displaced pelvic/hip fractures.
- ◼
Foreign bodies, such as bullet fragments, which could preclude future magnetic resonance imaging (MRI).
- ◼
- ◼
Insensitive to most organ or soft tissue injuries and detection of hemorrhage.
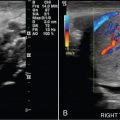
Ultrasonography
- ◼
Rapid and portable. Good for intraabdominal hemorrhage detection and testicular trauma evaluation. Otherwise, role is limited because a comprehensive abdominopelvic evaluation is time consuming and requires a skilled sonographer. Ultrasound (US) is highly operator dependent.
- ◼
Focused assessment with sonography for trauma (FAST): Quick ultrasound protocol to detect hemorrhage in four locations: perihepatic/hepatorenal (right upper quadrant view), perisplenic (left upper quadrant view), pelvic (suprapubic view), and pericardial (subxiphoid view). Stable patients with positive FAST need a computed tomography (CT) scan. Not all clinically relevant injuries result in hemoperitoneum.
Computed tomography
- ◼
CT is widely available in the emergency setting and is the workhorse to assess abdominopelvic trauma because of rapid image acquisition (whole body in seconds) and sensitivity/specificity for hemorrhage, intraperitoneal free air, internal organ injury, vascular injury, and bony fracture.
- ◼
Intravenous contrast helps to identify vascular and solid organ injuries.
- ◼
Patient must be stable enough to travel to the CT scanner (unlike US or radiography).
Magnetic resonance imaging
- ◼
Typically used to answer a specific targeted question or follow up on known findings rather than serve as a screening test for injuries, for example:
- ◼
Presence of radiographically occult hip fracture.
- ◼
Assessment of spinal trauma.
- ◼
Assessment of pancreatic or biliary injury.
- ◼
- ◼
Limitations: long examination times, patients must be hemodynamically stable, not portable, limited availability (especially in the emergency setting), and patient specific contraindications (i.e., unknown metallic foreign body, MRI unsafe device). MRI is insensitive to key findings, such as intraperitoneal free air or pneumothorax (unlike CT).
Protocols
Protocol considerations
Computed tomography
- ◼
Oral contrast: not routinely administered. Increased risk of aspiration. Patients may be unable to ingest contrast because of injuries. May delay diagnosis of life-threatening injuries.
- ◼
Intravenous contrast (typical volume 100–150 cc).
- ◼
Not required to detect hemoperitoneum or other hemorrhage (but required for diagnosis of active bleeding).
- ◼
Crucial for evaluation of the vasculature, solid organs, and urinary system.
- ◼
Optimal image quality requires careful timing. Multiphase imaging often needed.
- ◼
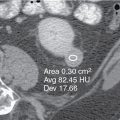
Angiographic phase (25–30s delay) for vessel evaluation.
- ◼
Portal venous phase (65–80s delay) for intraabdominal organ assessment.
- ◼
Delayed phase (5–10 min delay) to distinguish contrast extravasation from pseudoaneurysm (early delay) or for urinary tract injuries (late delay).
- ◼
- ◼
- ◼
Intravesical contrast: instill at least 300 cc of dilute contrast via Foley catheter into the bladder using gravity drip 40 cm above patient to evaluate suspected bladder injury.
- ◼
Radiation dose.
- ◼
Use sufficient radiation to diagnose injuries. Use the lowest dose that still provides diagnostic image: the ALARA (as low as reasonably achievable) principle.
- ◼
Radiation dose reduction with automated tube current modulation, iterative reconstruction, and delayed imaging only when portal venous phase lesion exists.
- ◼
Magnetic resonance imaging
- ◼
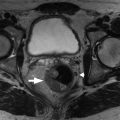
Fracture assessment includes a combination of noncontrast T1-weighted and fluid sensitive (STIR or fat suppressed T2-weighted) images in multiple planes. Spine imaging uses additional gradient echo T2*-weighted (for hemorrhage) and diffusion-weighted imaging (for cord injury) images.
- ◼
Optimal MRI protocols for intraabdominal organ evaluation vary based upon the organ of interest. Intravenous contrast may be helpful depending upon the indication.
Sample abdominal computed tomography protocol
- ◼
Portal venous phase abdominopelvic CT without oral contrast.
- ◼
Delayed phase (5–10 minute) CT if injury is identified on portal venous phase.
- ◼
Subsequent CT cystogram for concern of bladder injury.
- ◼
Multiplanar image reconstruction; 2.5 to 5 mm slice thickness in soft tissue and bone kernel.
- ◼
Consider separate arterial phase acquisition or split phase contrast injection with combined arterial/portal venous phase acquisition.
Specific disease processes
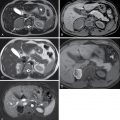
Hepatobiliary trauma ( figs. 38.1–38.3 )
- ◼
Active extravasation in stable patients requires diagnostic angiography and embolization.
- ◼
Most isolated liver injuries are managed nonoperatively unless the patient is unstable.
- ◼
Isolated gallbladder injury is uncommon. Findings are nonspecific: decompressed gallbladder, pericholecystic fluid, and gallbladder wall thickening.
- ◼
Blunt injury to the extrahepatic bile ducts is rare. The major complication is bile leak.




Splenic trauma ( figs. 38.4–38.6 )
- ◼
Most frequently injured organ in abdominal blunt trauma.
- ◼
Injury can lead to large volume hemoperitoneum and hemodynamic compromise.
- ◼
Most injuries are managed nonoperatively. Active extravasation, large volume hemoperitoneum, pseudoaneurysm, and arteriovenous fistula predict failure of conservative management. Endovascular treatment preferred over surgery.
- ◼
Delayed postcontrast CT distinguishes pseudoaneurysm from active extravasation.
- ◼
Sentinel clot sign: with large volume hemoperitoneum and multiple solid organ injuries, it is a challenge to identify a bleeding source. Densest blood (sentinel clot) resides near the bleeding source (see Fig. 38.4 ).



Pancreatic trauma ( fig. 38.7 )
- ◼
Severe mechanism of injury is required; isolated pancreatic injuries are rare.
- ◼
Pancreatic body is most vulnerable to injury, most commonly from crush mechanism.
- ◼
Pancreatic duct injury: main cause of morbidity/mortality. Treat with surgery or endoscopy.
- ◼
Clinical findings (leukocytosis, elevated serum amylase, abdominal pain) may not present for a few days. Imaging findings are often subtle!
- ◼
Look for pancreatic laceration (thin hypoenhancing band through the pancreatic parenchyma) of greater than 50% of pancreatic width to suggest duct injury.
- ◼
Consider magnetic resonance cholangiopancreatography to characterize.