Anatomy, embryology, pathophysiology
- ◼
The adrenal glands are multifunctioning, inverted Y-shaped, retroperitoneal endocrine glands normally located superior to the kidneys in the perirenal space ( Fig. 28.1 ).
- ◼
The adrenal glands mediate the stress response by releasing cortisol and are involved in secondary sex hormone synthesis and blood pressure regulation.
- ◼
Absence of the Y-shape indicates development in the absence of an orthotopic kidney (i.e., agenesis or ectopia).

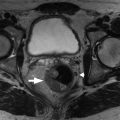
Fig. 28.1
Normal adrenal glands. The axial T2-weighted image (A) shows normal bilateral adrenal glands ( arrows ) as thin, linear, hypointense Y-shaped structures. The corresponding coronal T2-weighted image (B) shows the normal position of the adrenal glands surrounded by retroperitoneal fat and their relationship to the kidneys. The out-of-phase (C) and in-phase (D) images demonstrate some out-of-phase signal loss as a result of the presence of fat-containing enzymes and enzymatic precursors. The T1-weighted, fat-suppressed, postcontrast image (E) shows normal avid early adrenal enhancement.
(From Roth C, Deshmukh S. Fundamentals of Body MRI , ed 2. Philadelphia: Elsevier; 2016.)
- ◼
- ◼
The histological zonal architecture of the adrenal gland is divided into two distinct components: the cortex, which is derived from mesothelium, and the medulla, which is derived from neural crest cells.
- ◼
The adrenal cortex is composed of the zona glomerulosa, zona fasciculata, and zona reticularis.
- ◼
The superficial zona glomerulosa is the primary site of aldosterone production.
- ◼
The middle zona fasciculata synthesizes glucocorticoids (cortisol and corticosterone).
- ◼
The inner zona reticularis produces androgens.
- ◼
Adrenal cortical masses include adrenal adenoma, adrenal cortical carcinoma, adrenal myelolipoma, adrenal cysts, and metastasis.
- ◼
Adrenal hemorrhage can involve the cortex.
- ◼
- ◼
The adrenal medulla is in the centermost portion of the gland and is responsible for catecholamine production.
- ◼
Adrenal medullary masses include pheochromocytoma, neuroblastoma, ganglioneuroma, or ganglioneuroblastoma.
- ◼
- ◼
- ◼
Arterial blood supply is via the superior adrenal artery (via phrenic artery), middle adrenal artery (via abdominal aorta), and inferior adrenal artery (via renal artery).
- ◼
The left adrenal vein drains to the left renal vein and the right adrenal vein drains to the inferior vena cava (IVC).
Techniques
Computed tomography
- ◼
Primary modality for evaluating adrenal adenoma
- ◼
Adrenal glands enhance after iodinated contrast administration to approximately 50 to 60 Hounsfield units (HU).
- ◼
Both unenhanced computed tomography (CT) and dynamic contrast-enhanced CT have a role.
- ◼
Benign adenomas and malignant masses show rapid contrast enhancement, but adenomas demonstrate rapid washout of contrast.
Magnetic resonance imaging
- ◼
Alternative to CT when contrast-enhanced CT is contraindicated.
- ◼
Normal adrenal has low to intermediate signal on both T1- and T2-weighted imaging.
- ◼
Chemical shift imaging with T1-weighted gradient echo (GRE) sequences can be used to evaluate for microscopic fat in nodules (see Physics Pearls box).
- ◼
Frequency selective fat saturation can be used to determine presence of macroscopic fat in nodules.
Ultrasonography
- ◼
Normal adult adrenal glands are not seen on ultrasound. Incidental masses near the superior renal poles may be adrenal in origin.
- ◼
Can be used in pediatric evaluation.
Nuclear medicine
- ◼
Malignant adrenal lesions typically demonstrate 18-Fluoride deoxyglucose (18-FDG) uptake exceeding that of normal liver.
- ◼
Whole body 123-Iodine scintigraphy with metaiodobenzylguanidine (MIBG) compounds can detect functional lesions and is superior to other modalities in the detection of extraadrenal lesions.
- ◼
For patients with suspected pheochromocytoma (i.e., elevated urine catecholamine breakdown products) and negative MIBG scintigraphy, FDG-positron emission tomography (PET) or PET/CT may be useful.
Protocols
Suggested computed tomography protocols
- ◼
Unenhanced CT.
- ◼
An adrenal nodule measuring less than 10 HU can be reliably diagnosed as a benign adenoma (98% specific), unless greater than 4 cm ( Fig. 28.2 ).

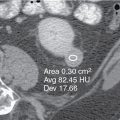
Fig. 28.2
An incidentally discovered left adrenal nodule has measured attenuation values of less than 10 Hounsfield units on unenhanced imaging. This is consistent with a lipid-rich adenoma.
(From Zagoria RJ, Brady CM, Dyer RB. Genitourinary Imaging: the Requisites , ed 3. Philadelphia: Elsevier; 2016.)
- ◼
- ◼
Adrenal washout CT.
- ◼
Absolute washout protocol: noncontrast, venous phase, and delayed phase (15 minutes) imaging.
- ◼
Absolute Washout=HUv–HUdHUv–HUn
Absolute Washout = HU v – HU d HU v – HU n
, where HU n , HU v , and HU d are the HU of an region of interest (ROI) in the nodule on noncontrast, venous phase, and delayed phase imaging, respectively.
- ◼
Absolute washout over 60% is diagnostic of benign adenoma, unless greater than 4 cm in size ( Fig. 28.3 ).

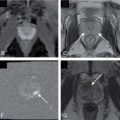
Fig. 28.3
Contrast material washout in an adrenal adenoma. A, Unenhanced computed tomography (CT) scan shows a homogeneous low-attenuation adrenal nodule with attenuation of 6 Hounsfield units (HU) (typical of a lipid-rich adenoma). B, On the portal venous phase of contrast enhancement, the nodule enhances with attenuation values of 86 HU. C, On 15-minute-delayed CT, the mass has decreased enhancement with attenuation of 32 HU. The contrast enhancement during the portal venous phase washed out by 68% by the time of the delayed scans, confirming that this is an adenoma. Absolute washout of 60% or greater is diagnostic of an adenoma.
(From Zagoria RJ, Brady CM, Dyer RB. Genitourinary Imaging: the Requisites , ed 3. Philadelphia: Elsevier; 2016.)

- ◼
Determination of benignity after noncontrast acquisition may negate need to complete postcontrast series.
- ◼
- ◼
Relative washout CT.
- ◼
Relative Washout=HUv–HUdHUv
Relative Washout = HU v – HU d HU v
.
- ◼
Relative washout over 40% is diagnostic of benign adenoma, unless greater than 4 cm in size.
- ◼
This protocol can be performed if there is concern for radiation exposure.
- ◼
Suggested magnetic resonance imaging protocols
- ◼
Chemical shift imaging protocol.
- ◼
Uses in-phase and opposed-phase T1-weighted GRE.
- ◼
Adenomas will demonstrate signal dropout from microscopic fat.
- ◼
Other lesions containing microscopic fat (e.g., well-differentiated adrenocortical carcinoma, clear cell renal cell carcinoma, and hepatocellular carcinoma) may also demonstrate signal dropout on opposed phase imaging.
- ◼
- ◼
Fat suppression can be used to demonstrate macroscopic fat as seen in myelolipoma.
Specific disease processes
Patterns of adrenal gland enlargement ( fig. 28.4 ).
- ◼
Diffuse enlargement.
- ◼
Adrenal hyperplasia ( Fig. 28.5 ).
- ◼
Response to excess adrenocorticotropic hormone (ACTH) from any cause; typically results in Cushing disease or hyperaldosteronism.
- ◼
Glands are enlarged with adreniform shape.
- ◼
Differentiating diffuse hyperplasia from functioning adenoma in hyperaldosteronism has treatment implications. If imaging does not identify a nodule, adrenal vein sampling is performed.

Fig. 28.5
Computed tomography (CT) of adrenal hyperplasia in a hirsute female with elevated concentration of dehydroepiandrosterone in the urine. CT scans demonstrate normal shape and size of the right (A) and left (B) adrenal glands ( solid arrows ). The ipsilateral diaphragmatic crus ( open arrows ) is commonly used as an internal standard for normal adrenal size. The measured width of the normal adrenal limb ranges from 4 to 9 mm, and because of this variation, adrenal hyperplasia may not be distinguishable from a normal adrenal gland at imaging or at surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


- ◼
- ◼