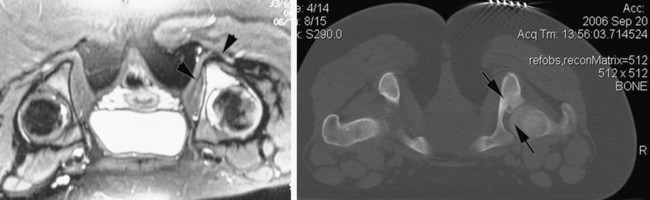
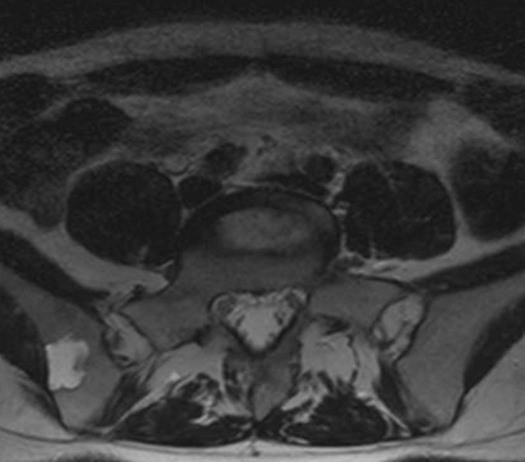
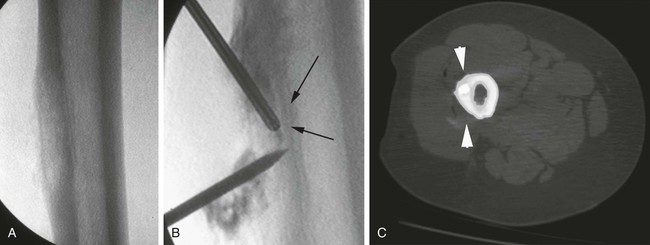
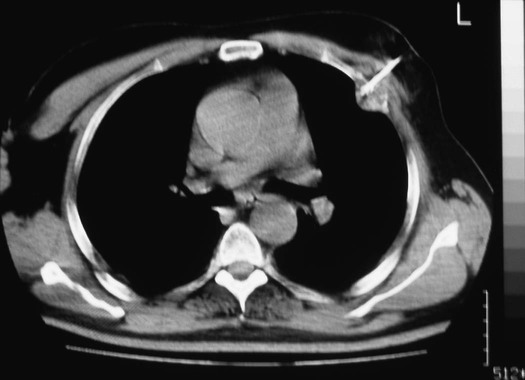
Alexis D. Kelekis, Jean-Baptiste Martin and Dimitrios Filippiadis Primary or metastatic bone disease can become very painful, especially in cases of lytic lesions. Possible treatments include surgery, embolization, chemotherapy, radiotherapy, and palliative analgesics.1 Hypoxic cells with limited blood flow can be resistant to chemotherapy and external beam radiation therapy. These cells may be more sensitive to ablation because of increased cell sensitivity to heat in hypoxic state and decreased heat dissipation due to poor tumor perfusion.2 External beam radiation, although used frequently, provides pain relief in only 70% of patients treated.3 Tumor destruction with ablation treatments, although fairly recent in its application within the musculoskeletal system, has evolved and seems effective for treatment of painful skeletal lesions. Such lesions can be treated by ablation, providing local tumor control either as a single-modality treatment or as an adjunct to surgical resection or other percutaneous techniques.4,5 Ablation can be curative for small lesions (up to 3-5 cm).6 In bigger lesions, its main purpose is palliative treatment and to provide local control of the disease via a percutaneous approach. It can also help diminish local spread into muscle and can be used in conjunction with other techniques (vertebroplasty, surgery, radiotherapy), especially when the size of the lesion undermines bone stability.6 Ablation can be very effective for lesions spreading in soft tissues, diminishing tumor burden and mass effect on other organs.7 Ablation inside bone, especially when the cortex is intact, can have an oven effect and completely destroy small lesions. The most common benign lesion treated with radiofrequency ablation (RFA) is osteoid osteoma5,8 (Fig. 158-1). Aneurysmal bone cysts can also be treated by RFA prior to filling, thus replacing the curettage technique (Fig. 158-2). In the treatment of malignant painful lytic lesions spreading into bone and muscle, ablation can help provide local tumor control. When the lytic lesion is in a weight-bearing structure (involving > 40% of healthy bone), ablation must be accompanied by bone-supporting techniques (vertebroplasty, osteoplasty, intraosseous stent or surgery) to avoid the risk of bone collapse under the induced osteonecrosis.6,7 Ablation can also help reduce the possible mass effect from the soft-tissue component of the lesion (Fig. 158-3). Patients must be able to withstand the percutaneous approach as well as the ablation. When the lesion is deep in the bone structures, irritation of the periosteum is minimal and so is the pain sensation. On the contrary, when the lesion involves muscle structures or affects the periosteum, sedation is mandatory. Usually the treatment can be performed under monitored assisted conscious sedation9,10 (Fig. 158-4). Absolute contraindications to ablation are the same as in any image-guided percutaneous procedure and include coagulopathy disorders, skin infection, immunosuppression, and absence of a safe path to the lesion without harming vital organs or structures.8 As noted earlier, bone radiofrequency can be very effective when cortical bone is intact, producing an oven effect. When there is a severe lytic lesion of the cortex, electrical impulses can spread out easily, thus affecting surrounding vital structures. Especially in the spine, when the metastatic lesion is affecting the posterior wall, monopolar ablation can affect the nerves in the spinal canal.7,11 In these cases, thermal monitoring of the epidural space can help prevent irreversible damage (Fig. 158-5). Injection of mediating solutions can help avoid damage of vital organs by either insulation or displacement of the structure one wishes to avoid.7,11 1. Monopolar systems require a grounding pad placed on the patient to “close” the electric circuit. Their main disadvantage is the formation of aberrant currents, which do not always allow for uniform energy deposition inside the lesion.12 They can be divided into single electrode and multitined electrodes and are the most frequently used devices. Single electrodes have the advantage of small caliber but have smaller ablation radius. Different kinds of single monopolar devices exist to amplify treatment size. They can feature hot, cooled-tip, and water-perfused electrodes and work independently or in cluster mode. Depending on the type of electrode, the ablation shape changes. Multitined electrodes increase energy deposition by creating larger zones of coagulation and produce better lesion destruction.2 There are three RFA systems available with expandable needle electrodes. The three systems differ in needle electrodes, generators, and the algorithms used to maximize coagulation volumes. 2. Bipolar devices do not require a grounding pad, because the current passes through the same or neighboring needles, thus diminishing the risk of aberrant currents. The distance between the electrodes can be variable depending on the type of needle used.13,15 3. Coblation is a controlled non–heat-driven process. It uses radiofrequency energy to excite the electrolytes in a conductive medium (e.g., saline solution), creating precisely focused plasma. The plasma’s energized particles have sufficient energy to break molecular bonds within tissue, causing it to dissolve at relatively low temperatures (typically 40°C-70°C). The result is volumetric removal of target tissue.14 Microwave ablation (MWA) is a relatively recent ablation mode that delivers cytotoxic effects and cellular death by means of coagulation necrosis. Microwave antennae are inserted within the tumor and transmit high-frequency energy that facilitates molecular movement and frictional forces, resulting in temperature elevation and subsequent necrosis.16 With MWA, a larger ablation zone is created within a shorter period of time. The applied energy extends approximately 2 cm around the antenna and not throughout the whole body as in RFA. The ablation zone is not governed by the heat sink effect produced by nearby vessels, and in contrast to RFA, no grounding pads are necessary. All the aforementioned factors make MWA the treatment of choice for large tumors in close proximity to a vessel.17 Technical parameters of the ablation session are determined by the manufacturer of the antenna. In most protocols, 5 to 10 minutes of ablation is performed at 40 to 60 watts. When choosing appropriate therapeutic protocol, one must balance killing all malignant cells against minimizing surrounding tissue damage. A safety margin of 5 to 10 mm is mandatory for MWA. In selected cases, multiple antennae can be applied simultaneously, depositing energy in a synergistic fashion, which will result in even larger ablation zones. Cryoablation is the application of extreme cold to destroy tumor cells by means of both direct cellular and vascular injury. In contrast to other ablation types, up to 25 probes can be used within the same lesion (depending on lesion size). In cases of multiple placements, probes should be more or less parallel and about 2 cm apart.18
Ablation and Combination Treatments of Bony Lesions
Clinical Relevance
Indications
Contraindications
Equipment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine