Acute pelvic pain in the female patient is usually caused by inflammation or infection of the gastrointestinal or genitourinary organs. Forging a differential diagnosis based on physical findings and symptomatology can be exceedingly difficult, particularly in patients with obesity or chronic disease of the pelvic structures. Imaging is of great value in directing the physician to the organ of interest and determining therapy. A focused differential diagnosis of acute pelvic pain includes ovarian or tubal infection including abscess, ovarian torsion, hemorrhagic or ruptured ovarian cyst, inflammatory bowel disease such as Crohn’s disease or ulcerative colitis, appendicitis, diverticulitis, and renal colic. Less common pathology includes perforation of the uterus by an intrauterine device (IUD) and dilation of an endometrioma resulting from internal hemorrhage. It is important for both the referring physician and radiologist to remember that acute pelvic pain is not always caused by ovarian disease.
Disease
Definition
- 1.
Pelvic inflammatory disease (PID) is inflammation of the upper genitalia (endometrium, fallopian tubes, and ovaries) and the adjacent pelvic region.
- 2.
Ovarian torsion is defined as partial or complete rotation of the ovarian vascular pedicle causing obstruction to venous outflow and arterial inflow.
- 3.
Ectopic pregnancy is a viable fetus located outside the uterus, usually in the fallopian tube.
- 4.
Hemorrhagic ovarian cysts are common in women of menstrual age. When a large cyst ruptures, the blood products irritate the peritoneal surfaces.
- 5.
Inflammatory bowel disease is a heritable disorder that manifests with circumferential wall thickening and adjacent inflammation and, when perforation occurs, abscesses. In the case of Crohn’s disease, the area most frequently affected is the terminal ileum.
- 6.
Appendicitis occurs when fecal material or calcifications become trapped within the tubular appendix, leading to inflammation and sometimes rupture.
- 7.
Diverticulitis is caused by perforation of a colonic diverticulum, most commonly in the sigmoid colon.
- 8.
Renal colic is secondary to a stone lodged within the ureter, causing inflammation, obstruction of urine flow, and severe pain with peristalsis of the ureter.
- 9.
Fibroids are benign muscular tumors of the uterus that may bleed or undergo necrosis.
Prevalence and Epidemiology
It is difficult to estimate the prevalence of pelvic pain. Almost every woman has experienced it at least once in her lifetime. In the United States, approximately 1.5 million women are affected with PID every year. Frequency of ovarian torsion is highest in the reproductive age group with a few cases seen in children and postmenopausal women. Adnexal torsion is the fifth most common gynecologic emergency condition with a prevalence of 2.7%.
Etiology and Pathophysiology
Pelvic Inflammatory Disease
The etiologic agent is often never identified, but Chlamydia trachomatis , Neisseria gonorrhoeae , and aerobic and anaerobic vaginal flora (including organisms involved in bacterial vaginosis) are known to be the cause in some cases. Sexually transmitted diseases like chlamydia and gonorrhea account for one third to one half of PID infections. Risk factors include young age, high frequency of partner change, lack of barrier contraception, low socioeconomic group, and smoking. Risks associated with IUD insertion have been shown to be limited to the 4 weeks after insertion in women at low risk for sexually transmitted infections.
Ectopic Pregnancy
Tubal pregnancy has become more common as a result of the high prevalence of PID and increasing use of infertility treatments. A woman with a positive pregnancy test and no intrauterine pregnancy likely has an ectopic pregnancy. The most common location is the ampullary portion of the fallopian tube. As the fetal sac increases in size, pain and rupture will occur. Absence of an intrauterine pregnancy with a mass adjacent to the ovary is virtually diagnostic of ectopic pregnancy. Blood within the cul-de-sac is a common feature.
Ovarian Torsion
Multiple factors have been found to be responsible for the development of ovarian torsion. Most patients with ovarian torsion have pathology in the involved ovary or tube that likely causes abnormal twisting. Most frequent pathologic findings with adnexal torsion include benign cystic teratomas, hemorrhagic or follicular cysts, and cystadenoma; however, paratubal cysts or hydrosalpinx may also cause torsion. Torsion in a normal ovary is rare and is most common among young children, in whom developmental abnormalities such as long fallopian tubes or absent mesosalpinx may be responsible. Other etiologies for adnexal torsion include adnexal venous congestion resulting from constipation, sigmoid distension, or pregnancy.
Hemorrhagic Cysts
All ovulating women will develop ovarian cysts. In the majority of cases, a dominant follicle develops in preparation for ovulation. Pain with ovulation may occur 10 to 12 days after the onset of menstruation. Occasionally a cyst fails to rupture or is associated with localized bleeding. The dilated, blood-filled cyst causes pressure and pain. When rupture occurs, the majority of patients will feel relief, although occasionally a large volume of blood will cause irritation of the peritoneal surfaces and continued pain.
Inflammatory Bowel Disease
Crohn’s disease usually manifests during the third decade of life with abdominal pain, diarrhea, and systemic symptomatology, including fever and perianal abscess. This is likely a heritable disease because it is more common in those of Semitic descent, although it has been reported to occur in all races. Circumferential and transmural wall thickening can involve any portion of the gastrointestinal tract but most commonly the terminal ileum. On endoscopy, transmural inflammation and the presence of crypt abscesses are diagnostic of Crohn’s disease.
Appendicitis
Roughly 10% of Americans will suffer appendicitis during their lifetimes. The appendix, a narrow tubular structure arising from the tip of the cecum, likely has no current gastrointestinal function. Inflammation of the wall and occlusion of the orifice lead to the classic presentation of right lower quadrant pain, obstipation, and vomiting. Left unchecked, most cases will proceed to rupture and abscess formation.
Diverticulitis
This disease occurs most commonly in middle-aged and elderly populations. Over time, peristalsis of the colon leads to the development of pulsion diverticula at weak points in the colonic wall. When one of these diverticula becomes obstructed, a small perforation occurs, leading to severe colonic inflammation and wall thickening. Abscess formation is a common complication.
Renal Colic
Formation of renal stones is extremely common, particularly in those living in the southeastern United States. In most cases the cause of stone development is unknown, but diet is thought to play a part. Even small stones can irritate the ureteral wall, causing inflammation and proximal dilation of the ureter and hydronephrosis.
Fibroids
Fibroids are common and present in approximately 40% of women. Although many women suffer little symptomatology, some have severe pain, bleeding, and bowel and bladder problems.
Manifestations of Disease
Clinical Presentation
Virtually all the diseases listed above present with pelvic pain, often accompanied with nausea and vomiting. Location of the pain can sometimes be helpful, such as appendicitis in the right lower quadrant and diverticulitis in the left; however, referred pain is common, and usually abdominal examination is inadequate to identify exact origin. On pelvic examination, cervical motion tenderness is virtually diagnostic of PID. Severe episodic pain extends from the flank with renal colic. Fever is common to all infectious processes, including diverticulitis and appendicitis, particularly when rupture or abscess formation occurs. The presence of a perianal abscess is a strong predictor of Crohn’s disease.
Imaging Indications and Algorithm
A woman with unstable vital signs or an acute abdomen on physical examination should be taken to the operating room. In a stable patient, ultrasound (US) is the test of choice for imaging the pelvis. US is accurate in the identification of virtually all diseases arising from the gynecologic organs and has no ionizing radiation. When US is negative, computed tomographic (CT) scan with oral and intravenous contrast media should be performed. Magnetic resonance imaging (MRI) is usually reserved for cases in which CT is nondiagnostic.
Imaging Technique and Findings
Radiography
Radiography is not routinely helpful in imaging of the pelvis outside of trauma. Plain films may be helpful to diagnose bowel obstruction, locate a foreign body, and identify calcifications including appendicoliths and renal stones.
Ultrasound
US is the test of choice for the diagnosis and evaluation of pelvic pain. It can be performed transvaginally or transabdominally; the transvaginal approach provides more detail, whereas transabdominal imaging provides a larger field of view ( Figure 10-1 ). It is essential that the uterine fundus be seen in its entirety to identify pedunculated fibroids. Images showing the iliac vessels are important to exclude adnexal masses abutting the pelvic sidewall. US can also be used to guide abscess drainage.

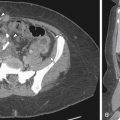
Pelvic Inflammatory Disease
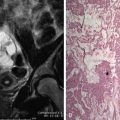
In the early stages of PID, US may be normal, and hence a normal US in a patient with clinical suspicion of PID does not exclude the diagnosis. The presence of free fluid in the cul-de-sac or pouch of Douglas (see Figure 10-1 , B ) is also not a specific sign of PID and may be present in other conditions such as follicular rupture, ovarian cyst, malignancy, or ectopic pregnancy, in addition to other nongynecologic causes of fluid. Fifty percent of patients with PID may demonstrate free fluid in the cul-de-sac that appears anechoic and may be small in quantity. With inflammation, there is dilation of the tube with formation of a hydrosalpinx or pyosalpinx. As the disease progresses, the ovary can become involved and enlarges with loss of corticomedullary distinction. When the ovary adheres to the tube, it forms a tuboovarian complex. A tuboovarian abscess (TOA) is caused by complete breakdown of ovarian and tubal architecture without the ability to differentiate them. TOA may appear as a homogenous, hypoechoic cystic mass or a mass containing mixed echogenicity areas ( Figure 10-2 ). Septae within this mass may appear thickened and asymmetric.

Ovarian Torsion
The spectrum of reported imaging findings in torsion varies as a result of the degree and duration of adnexal torsion. If the torsion is incomplete, massive ovarian edema may result ( Figure 10-3 , A ); however, with increasing degree of obstruction, there is complete lack of flow to the ovary, and the ovary may be normal size but without any flow in it. With torsion, however, a large ovary is the most constant finding in multiple previous articles with the enlargement caused by either the edema or a mass.

Other findings seen on gray scale imaging include hyperechoic central areas of edema and peripherally placed follicles and large cystic mass with internal debris. The color and spectral Doppler findings in ovarian torsion are also highly variable and are based in part on the degree of vascular compromise. The classic finding of absent ovarian arterial flow is seen in only 73% of cases, and some cases may even have a normal color Doppler flow to the ovary. Venous flow abnormality, however, is the most frequent finding with either decreased or absent venous flow seen in 93% of cases. Other findings include a twisted vascular pedicle sign and the whirlpool sign. The twisted vascular pedicle sign is the rotation site of the vascular pedicle itself and is seen as an echogenic round or beaked mass with multiple concentric hypoechoic and target-like stripes. Visualization of the circular or coiled vessels within this twisted pedicle on color Doppler is the whirlpool sign.
Ectopic Pregnancy
Normal findings of a developing intrauterine pregnancy on transvaginal US (TVUS) are an intrauterine gestational sac at 5 weeks, yolk sac at 5.5 weeks, and fetal heart motion at 6 weeks. When these findings are absent in the presence of a positive pregnancy test, an early pregnancy, spontaneous abortion, or ectopic pregnancy should be considered. The most specific appearance of an ectopic pregnancy is a thick-walled cystic mass adjacent to the ovary ( Figure 10-4 ). A dilated fallopian tube, fetal pole, and blood in the cul-de-sac are other common findings. Even with a normal appearance, ectopic pregnancy is present in up to one third of cases. Serial β–human chorionic gonadotropin (hCG) examinations are useful to follow the course of a possible ectopic pregnancy.

Hemorrhagic Cysts
Blood within a cyst changes in appearance with age. In the acute phase, hemorrhage is brightly echogenic with minimal through-transmission. As the hemorrhage evolves, more anechoic fluid is seen centrally, although a thick vascular rim may remain. Mature hemorrhagic cysts contain gracile septa within a thin rim ( Figure 10-5 , A ). In the case of endometrioma, the classic appearance is that of a cyst containing shifting echoes indicative of blood products ( Figure 10-5 , B ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree