Administration of Contrast Agents
Contrast-Enhanced CT-Scans and Contrast Media
To achieve high-image quality for diagnostic approaches, radiologists perform most CT-examinations as contrast-enhanced scans. Only a minority of CT-exams (e.g., stone protocols, fracture assessments) are noncontrasted scans (i.e., without CM-application). In developed industrial countries, the preferred and most used contrast materials are iodinated and nonionic contrast media. These agents are water-soluble derivatives of the triiodobenzoic acid, and are of low osmolality.
Per Oral CM-application
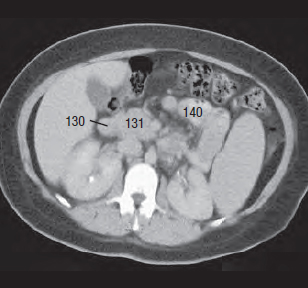
In addition to intravenous contrast, the examination of the GI-tract needs per oral CM-application. Without such contrast, it is difficult or impossible to differentiate between the duodenum (130), and the head of the pancreas (131 in Fig. 20.1 ).
Moreover, the differentiation between other GI parts (140) and neighboring structures could be also impossible. Following per oral contrasting, we can well delineate both the duodenum and the pancreas ( Fig. 20.2a, b ).
In contrast to the intravascular CM-application, we can use both low- and high-osmolar iodinated CM for the per oral application. Patients without any risk for an aspiration can receive a high-osmolar iodinated contrast medium (e.g., Gastrografin®), and patients at risk should receive a low-osmolar iodinated contrast medium (e.g., Ultravist®). One should be aware that the same precautions as mentioned below for intravenous contrast applications should also be used for the per oral application [18a].


The Procedure
Following a period of fasting (the day of the examination), the patient should drink an iodinated contrast medium in small portions over a period of 20–60 minutes before the CT examination starts. Therefore, the patient should arrive on time for an abdominal CT examination. To contrast the proximal GIT, the patient should drink the contrast agent 20–30 minutes before the CT scan starts. However, if the entire colon and the rectum will be scanned, it is recommended that the patient drinks the contrast medium approximately 45–60 minutes before the CT scan starts. In order to scan pelvic organs (e.g., bladder, cervix, or ovary), an additional rectal application of 100–200 ml iodinated contrast medium is necessary to differentiate tumors clearly from parts of the colon, sigmoid, or rectum, for example. To achieve complete contrast of the whole GIT, dilute Gastrografin® 1:3 up to 1:4 in water. If the upper part of the GIT should be examined only, use a reduced volume of diluted Gastrografin®.
If the urinary bladder has been removed and replaced by an ilial-conduit, initially the abdomen should be scanned by using an intravenous applied contrast agent only, which is excreted along with the urine in the conduit but not via the intestine. If necessary, a second scan with oral contrast may follow to delineate the intestine. Other protocols use mannitol and water, for example [18b].
Additional Medication for an Optimal Imaging Result
For an optimal assessment of the stomach walls, plain water is increasingly used as a hypodense contrast agent in combination with intravenous Buscopan® (scopolamine butylbromide), which relaxes muscles in gastric and bowel walls and thus reduces peristaltic movements [18c].
Intravenous CM-Application
Most commonly, we apply contrast materials as intravenous injection by using an automated power injector. We calculate the CM-dose on both the body weight, and the necessary diagnostic procedure: examinations of the neck or of an aortic aneurysm (to exclude a dissection flap), require higher concentrations than cranial CT-scans, for example. Usually, a CM-dose (e.g., iopromide) of 1.2 mL/kg body weight leads to excellent image results.
An increase in the density of blood vessels not only demarcates them better from muscles and organs but also provides information on the rate of blood perfusion (contrast agent uptake) in pathologically altered tissues: disturbances of the bloodbrain barrier, the borders of abscesses, or the inhomogeneous uptake of contrast agents in tumorlike lesions are only some examples. We call this phenomenon contrast enhancement: the contrast agent increases, i.e., the density and thus the signal is intensified. Depending on the patient’s health problem and an unenhanced (plain) scan should be obtained initially, followed by the intravenous injection of the contrast agent. We can more easily detect vascular grafts, inflammatory processes within bones, and abscess walls, if we compare unenhanced and contrast-enhanced images. The same holds true for focal liver lesions examined by using conventional CT techniques. Helical CT allows serial liver images in the early phase of arterial contrasting, followed by a series in the phase of venous drainage [17]. This procedure even allows the detection of small focal lesions (see pp. 121–124).
Preparing the i.v. Line
The injected bolus of contrast is modified when passing through the pulmonary circulation. The injection should therefore ideally have a rapid flow rate of 2–6 mL/sec for achieving sufficient density enhancement of the blood vessels [29]. A Venflon® canula with a diameter of at least 1.0 mm (20G), or preferably 1.2–1.4 mm (18G–17G), is used. Checking that the canula is correctly in the vessel is essential. A trial injection of sterile saline into the vein at a high flow rate should be carried out before injecting contrast agents. The absence of subcutaneous swelling confirms proper positioning: Thus, the fact that the vein can accommodate the intended flow rate can also be confirmed.
Inflow Phenomena
The streaming artifact of enhanced and unenhanced blood results from a short time interval between the start of injection and the onset of data acquisition. Since inflow is usually from one side via the axillary, subclavian, and brachiocephalice veins (91) into the superior vena cava (92), there is an apparent filling defect within the vena cava ( Figs. 21.1a–21.3b ).
Knowing about such inflow phenomena avoids a false positive diagnosis of venous thrombosis. Using too high concentrations of contrast agents in this area could result in disturbing artifacts. More inflow phenomena are described on the next pages.






Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree