Cranial Pathology
After having discussed that partial volume effects due to asymmetric projections (i.e., 55b in Fig. 54.2b ) may be misinterpreted as acute hematomas, this chapter will point out the characteristics of the different types of intracranial hemorrhage.
Bleeding Caused by a Contusion
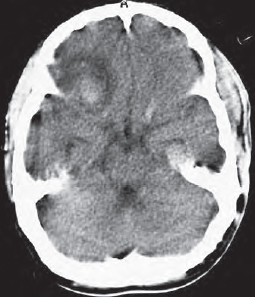
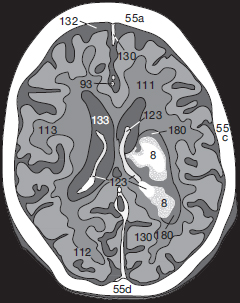
As a direct consequence of skull trauma, cerebral contusion bleeding may occur ( Fig. 54.1a ). An acute hemorrhage (8) appears as a hyperdense mass which may be accompanied by surrounding edema (180) and displacement of adjacent brain tissue. In anemic patients the hematoma is less dense and may therefore appear isodense to normal brain.
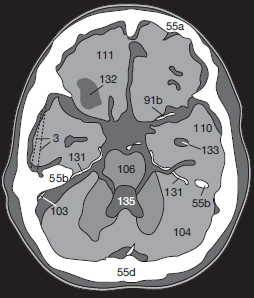
If the vascular wall is damaged only secondarily by hypoperfusion mediated by edema, hemorrhage may not occur until hours or, more rarely, days after skull trauma. A CCT obtained immediately after skull trauma which does not show any pathologic changes is therefore not a good predictor since delayed cerebral bleeding cannot be ruled out. A follow-up scan should be obtained if the patient’s condition deteriorates. After complete resorption of a hematoma ( Fig. 54.2a ), a well-defined defect isodense with CSF remains (132).
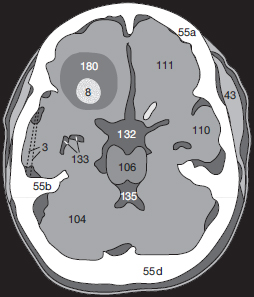
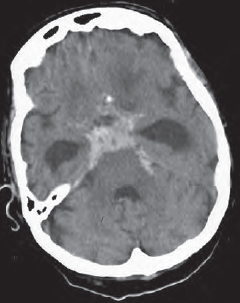
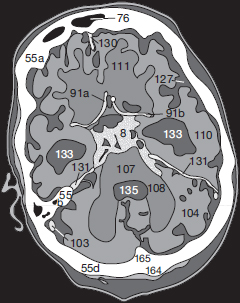
Contusion frequently leads to an epidural, subdural, or subarachnoid hemorrhage and may leak into the ventricles ( Fig. 55.1a ). Possible complications of such leakage or of a subarachnoid hemorrhage are disturbed CSF circulation caused by obstruction of the pacchionian granulations, the foramen of Monro, or of the 4th ventricle. An hydrocephalus with increased intracranial pressure and transtentorial herniation of the brain may result.
Epidural and subdural hematomas can also lead to major displacement of brain tissue and to midline shifts. Quite frequently this in turn causes obstruction of the contralateral foramen of Monro resulting in unilateral dilation of the lateral ventricle on the side opposite the bleeding (Fig. 56.3). The characteristics useful in differential diagnosis of the various types of intracranial bleeding are listed in Table 54.1 .
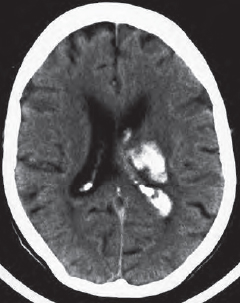
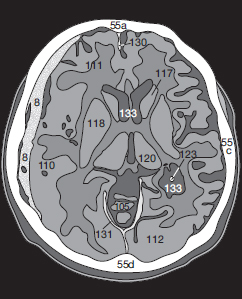
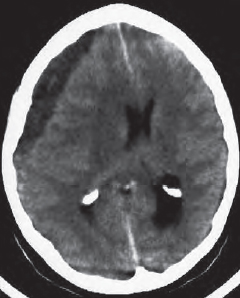
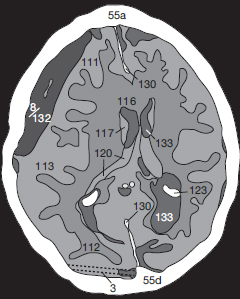
If there is intraventricular extension of intracranial hemorrhage ( Fig. 55.1a ), physiologic calcification of the choroid plexus (123), in the lateral (133) and 3rd ventricles (134), as well as those of the habenulae and the pineal (148), must be distinguished from fresh, hyperdense blood clots (8). Please note the edema (180) surrounding the hemorrhage ( Fig. 55.1a ).
If the patient has been lying supine, a horizontal fluid–fluid level caused by blood sedimenting in the posterior horns of the lateral ventricles may be seen ( Fig. 55.2a ). The patient is in danger of transtentorial herniation if the ambient cistern is effaced ( Fig. 55.2b ). In this case the 3rd ventricle is completely filled with clotted blood ( in Fig. 55.2a, b ), and both lateral ventricles are markedly dilated. CSF has leaked into the paraventricular white mater (). In addition, a lower section of this patient shows subarachnoid hemorrhage into the SAS (, in Fig. 55.2b ).

Subarachnoid Hemorrhage
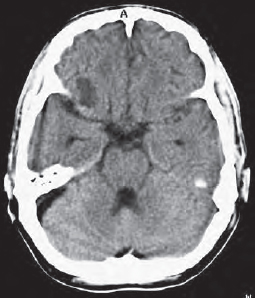
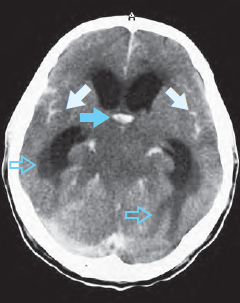
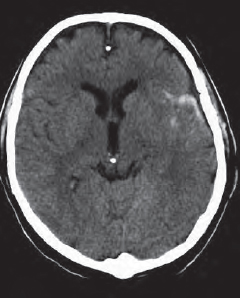
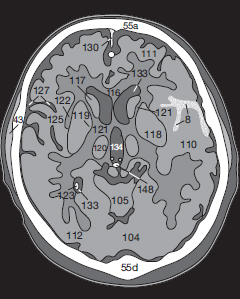
An obstructive hydrocephalus, as caused by subarachnoid hemorrhage (8 in Fig. 55.3a, b ), may easily be identified because the temporal horns (133) of the lateral ventricles appear distended. In such cases it is important to have a closer look at the width of the SAS over the cerebral surface: blunted cerebral gyri usually indicate a diffuse cerebral edema. In the present case though, the width of the Sylvian fissure (127) and the surface SAS are normal. Acute edema is therefore not present (yet).
Since the surface SASs are very narrow in younger patients, it is possible to miss a subarachnoid hemorrhage in children. The only identifiable sign may be a small hyperdense area adjacent to the falx (130). In adults a small subarachnoid hemorrhage also causes only a minor, circumscribed area of hyperdensity (8 in Fig. 56.1a ). At the time of this CT scan the bleeding was so slight that it had not yet caused any displacement of brain tissue.
Subdural Hematoma
Bleeding into the subdural space results from cerebral contusions, damaged vessels in the pia mater, or from torn emissary veins. The hematoma initially appears as a long, hyperdense margin close to the skull (8 in Fig. 56.2a ). In contrast to an epidural hematoma, it is usually somewhat irregular in shape and slightly concave toward the adjacent hemisphere. This kind of bleeding is not confined by cranial sutures and may spread along the entire convexity of the hemisphere.
Subdural hematomas can also cause marked displacement of brain tissue ( Fig. 56.3a ) and lead to disturbances in CSF circulation and to incarceration of the brain stem in the tentorial notch. It is therefore not as important, for treatment purposes, to distinguish between a subhematoma or an epidural hematoma as it is to ascertain the extent of the hemorrhage. Hematomas with the propensity to expand, especially if edema is a threat, should therefore be drained or treated surgically.

Chronic subdural hematomas (8 in Fig. 56.3a ) may appear homogeneously hypodense or show inhomogeneous density with sedimentation of blood. The danger involved in a small, venous bleed is the symptom-free interval and the slow onset of somnolence up to the development of a coma. Therefore, a patient with suspected bleeding after cranial trauma should always be kept under observation in order to detect any clinical deterioration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree