The adrenal glands are the primary focus of diagnostic attention in three clinical circumstances. A patient may be referred for imaging because a clinical diagnosis of adrenal hormone hyperfunction has been made. CT is then used to identify and characterize the lesion. The adrenal glands are commonly imaged to detect suspected metastatic disease, especially when the primary tumor, such as lung carcinoma, commonly metastasizes to the adrenal glands. Adrenal lesions are frequently detected incidentally on imaging studies performed for other indications (about 5% of all abdominal CT scans). The significance of the finding must be assessed radiographically and clinically. CT remains the imaging method of first choice for evaluation of the adrenal glands.
Normal Adrenal Glands
The adrenal glands have an outer cortex and an inner medulla that are functionally independent and anatomically distinct. The cortex secretes steroid hormones, including cortisol, aldosterone, androgens, and estrogens. The medulla produces the catecholamines epinephrine and norepinephrine. The adrenal glands lie in the perirenal space surrounded by retroperitoneal fat. The glands are usually triangular, or shaped like an inverted V or an inverted Y ( Fig. 16.1 ). The right adrenal gland lies above the right kidney posterior to the inferior vena cava between the right crus of the diaphragm and the right lobe of the liver. The left adrenal gland lies adjacent to the upper pole of the left kidney, posterior to the pancreas and splenic vessels and lateral to the left crus of the diaphragm. The limbs of the adrenal gland are 4 to 5 cm long and normally do not exceed 10 mm in thickness. Limb thickness is uniform, and the margins are straight or concave. Normal adrenal glands are about equal to muscle in CT attenuation on precontrast scans. Moderate enhancement is evident after contrast medium administration.

CT Technique for Adrenal Lesions
Noncontrast scans are obtained to document adrenal anatomy and to measure the precontrast attenuation of any lesions to serve as baseline attenuation for contrast enhancement. A slice thickness of 0.625 to 2.5 mm is used. The attenuation of any adrenal nodule or mass lesion is measured in the region of interest (ROI) that encompasses most of the lesion. If the average attenuation of the lesion is below 10 Hounsfield units (HU), the lesion is highly likely to be a benign adrenal adenoma. If the average attenuation of the lesion is above 10 HU, a contrast-enhanced study should be performed. Routinely 100 to 120 mL of nonionic contrast agent with an iodine concentration of 350 mg/mL is administered intravenously at 3.0 mL per second. Repeated thin-section scans (optimally 0.625 mm) through both adrenal glands are obtained at 60 seconds after contrast medium injection for the adrenal cortical phase and again at 15 minutes after contrast medium injection for the delayed phase.
Adrenal Lesions with a Specific Imaging Appearance
Myelolipoma
Myelolipoma is an uncommon benign adrenal tumor consisting of mature fat with interspersed hematopoietic bone marrow elements. The lesion is not associated with endocrine abnormalities and has no malignant potential. The tumor is most often discovered as an incidental finding. Occasionally tumors present with acute spontaneous painful hemorrhage. Tumors may also arise outside the adrenal gland.
- •
The presence of fat is characteristic. CT demonstrates large deposits of fat interspersed with higher-density soft tissue ( Fig. 16.2 ). The average fat attenuation within the tumor is –74 HU on unenhanced CT. The soft-tissue components are relatively low in CT attenuation (20–30 HU), reflecting the mixture of fat with the myeloid tissue.

FIG. 16.2
Myelolipoma.
A fat-density tumor (between arrowheads ) arises from the right adrenal gland. The streaks of soft-tissue density within the tumor represent hematopoietic bone marrow elements. A remnant of normal-appearing right adrenal gland (arrow) is evident. Note the low density of the lesion is the same as that of retroperitoneal fat (f) .
- •
Small calcifications may be present (24%).
- •
Hemorrhage alters the imaging appearance. CT shows acute hemorrhage as foci of high attenuation within the fatty mass. Size greater than 7 cm is associated with increased risk of hemorrhage. Surgical removal is recommended.
- •
Tumors range in size from 1 to 2 cm up to 17 cm. Growth of the lesion is reported in 50% of cases.
- •
Extra-adrenal myelolipomas are most common in the presacral space and retroperitoneum, occurring less commonly in the mediastinum, abdomen, and muscle fascia.
Cysts
True cysts of the adrenal gland are lined with endothelium or epithelium. Most lesions are asymptomatic and are discovered incidentally. They may produce symptoms because of hemorrhage.
- •
Cysts are well-marginated, thin-walled (<3 mm), nonenhancing, homogeneous, fluid-containing masses ( Fig. 16.3 ). Thin internal septations are sometimes present.

FIG. 16.3
True adrenal cyst.
A purely cystic mass (C) arises from the left adrenal gland (arrow) . No discernible cyst wall is evident. The internal density is homogeneously low and near to that of water in attenuation.
- •
The size may be up to 20 cm. The size of benign cysts may increase over time.
- •
The wall may have thin peripheral calcification if hemorrhage has previously occurred.
- •
Cyst contents have the characteristics of simple fluid (<20 HU) unless hemorrhage has occurred.
- •
Very rare parasitic cysts are usually caused by Echinococcus granulosus infection.
Pseudocysts
Pseudocysts account for about 40% of adrenal cysts. They occur as a sequela of previous adrenal hemorrhage. Pseudocysts have fibrous walls without a cellular lining.
- •
Pseudocyst appears as a hypodense mass with a thin or thick wall and, commonly, internal septations.
- •
Cyst contents are usually of higher attenuation than simple fluid, but cyst contents are not enhanced. Fluid-fluid levels may be present.
- •
Calcification in the wall is commonly present (56%) ( Fig. 16.4 ).

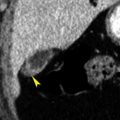
FIG. 16.4
Adrenal pseudocyst.
This cystic right adrenal gland mass (C) has calcification in a thin septation (arrow) and contains a coarse dense calcium deposit (arrowhead) . This appearance is characteristic of a posthemorrhage adrenal pseudocyst.
Adrenal Hemorrhage
Adrenal hemorrhage is common in the newborn and is caused by hypoxia, birth trauma, or septicemia. In older children and adults, hemorrhage is induced by blunt abdominal trauma, coagulopathy, or underlying tumor.
- •
On unenhanced CT, acute adrenal hemorrhage appears round or oval and hyperdense (50–90 HU) ( Fig. 16.5 ). Stranding is commonly present in the periadrenal fat.

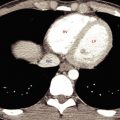
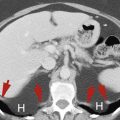
FIG. 16.5
Adrenal hemorrhage.
Postcontrast CT in a patient injured in a motor vehicle collision shows hemorrhage expanding the right adrenal gland (H) producing a homogeneous mass. Additional hemorrhage (arrows) is seen in the perirenal space. Follow-up CT 4 months later confirmed complete resolution of the adrenal hemorrhage.
- •
Posttraumatic adrenal hemorrhage has a marked predisposition to be unilateral on the right side as the right adrenal gland is compressed between the liver and the spine.
- •
With evolution and liquefaction of the blood clot, the adrenal mass shrinks and decreases in attenuation. Calcification of the hemorrhagic area may occur.
- •
Chronic changes of hemorrhage may be difficult to differentiate from other adrenal masses.
Pseudolesions
A variety of nonadrenal structures may simulate adrenal masses. Differentiation is made by having a high index of suspicion for pseudolesions and by performing appropriate correlative imaging tests. Accurate imaging diagnosis should obviously be made before adrenal biopsy. Pseudolesions are much more common on the left side because of the larger number of structures in the region of the left adrenal gland. Optimal CT technique with oral and intravenous contrast agents and multiplanar reconstructions makes confusion of pseudolesions with real adrenal lesions less likely.
- •
Unopacified portions of the stomach or small bowel are differentiated from an adrenal mass by administering oral contrast medium and repeating the CT scan ( Fig. 16.6 ).

FIG. 16.6
Adrenal pseudolesion.
(A) Initial CT scan revealing an apparent mass (arrow) in the region of the left adrenal gland. (B) Subsequent CT scan after administration of additional oral contrast medium showing contrast medium filling a gastric diverticulum (arrow) . A , Aorta; S , stomach filled with oral contrast medium; Sp , spleen.
- •
Tortuous blood vessels are identified by contrast-enhanced CT or Doppler ultrasound imaging. Splenic artery aneurysms often have a calcified wall and mimic a pseudocyst.
- •
An accessory spleen or a splenic lobulation is recognized by its smooth margin and by CT attenuation and enhancement identical to those of splenic tissue.
Adrenocortical Carcinoma
Primary carcinoma of the adrenal gland is rare, occurring in people aged 30 to 70 years. Adrenal carcinoma is associated with adrenal hyperfunction in 50% of cases. Cushing syndrome is most common. Other tumors present with abdominal pain or an abdominal mass. Most primary carcinomas are easily differentiated from adenomas by their imaging findings. The tumor is aggressive and highly lethal, with a strong propensity to invade blood vessels.
- •
The adrenal mass is usually large (>5–6 cm, average 12 cm) and markedly heterogeneous ( Fig. 16.7 ). A non–fat containing adrenal mass larger than 6 cm has an 85% chance of being malignant. Tumors usually replace the adrenal gland. Tumors are bilateral in 10% of cases.

FIG. 16.7
Adrenal carcinoma.
A huge solid heterogeneous mass (M) replaces the left adrenal gland. The pancreas (P) and stomach ( S ) are anteriorly displaced by the mass, confirming that the origin of the tumor is in the retroperitoneum.
- •
Central necrosis is common, and irregular calcification ( Fig. 16.8 ) is present in 30% of cases.

FIG. 16.8
Adrenal carcinoma with necrosis.
Postcontrast CT reveals a solid mass (M) arising from the right adrenal gland and invading the liver (arrowheads) . Extensive low attenuation within the mass is evidence of necrosis.
- •
Tumors enhance heterogeneously and have washout characteristics of malignant lesions ( Fig. 16.9 ). On unenhanced CT, tumor attenuation is greater than 10 HU.

FIG. 16.9
Adrenal carcinoma.
Coronal CT image showing a heterogeneously enhancing mass (arrowhead) arising from the left adrenal gland. A coarse calcification is present. The heterogeneous contrast enhancement and calculated relative percentage washout of 28% are characteristic of malignancy. LK , Left kidney; S , spleen.
- •
Tumor thrombus in the renal vein or inferior vena cava ( Fig. 16.10 ) is a frequent complication that carries a significant risk of pulmonary embolus.

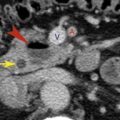
FIG. 16.10
Adrenal carcinoma invading the inferior vena cava.
A large solid tumor (Ca) replaces the right adrenal gland and invades the retroperitoneal fat (arrows) . The tumor extends into and enlarges the inferior vena cava (arrowhead) . A , Aorta.
- •
Direct invasion of adjacent structures and metastases to regional lymph nodes, liver, bone, and lung are common findings at presentation.
- •
Focal fat deposits are sometimes present in adrenal carcinomas. However, all fat-containing tumors reported have had other evidence of malignancy.
- •
Rarely, large degenerated benign adrenal adenomas have an appearance similar to that of adrenal carcinoma.
Lymphoma
The adrenal gland is involved in approximately 4% of patients with non-Hodgkin lymphoma. Primary lymphoma arising in the adrenal gland is extremely rare.
- •
Most common is total encasement of the adrenal gland by retroperitoneal adenopathy ( Fig. 16.11 ). The adrenal gland is often not visible.