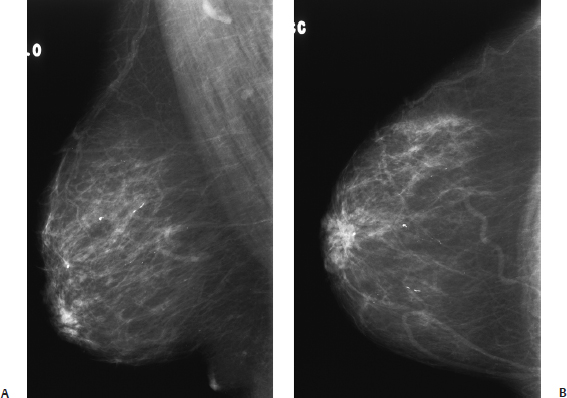
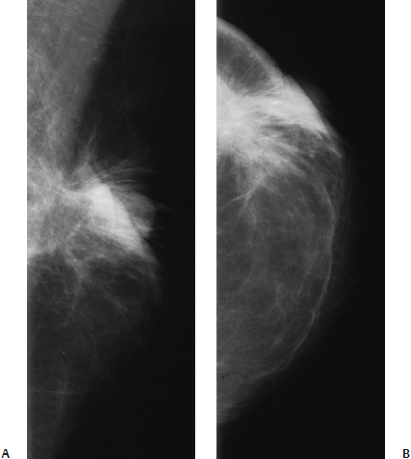
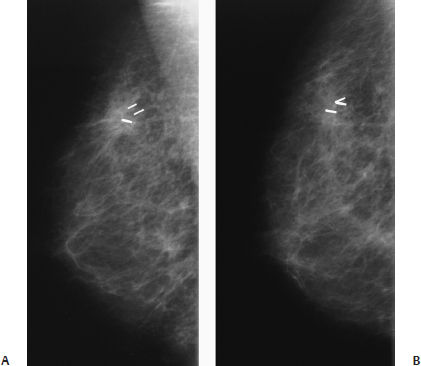
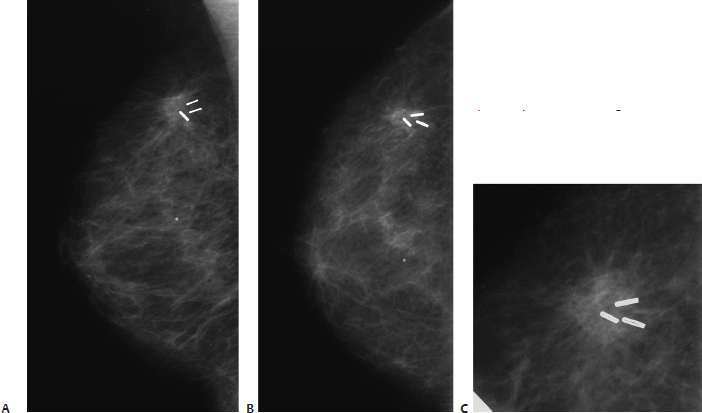
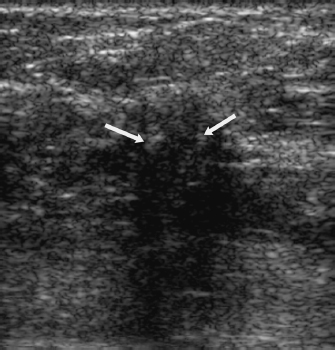
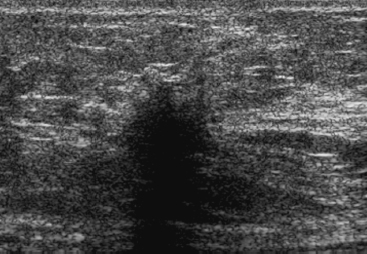
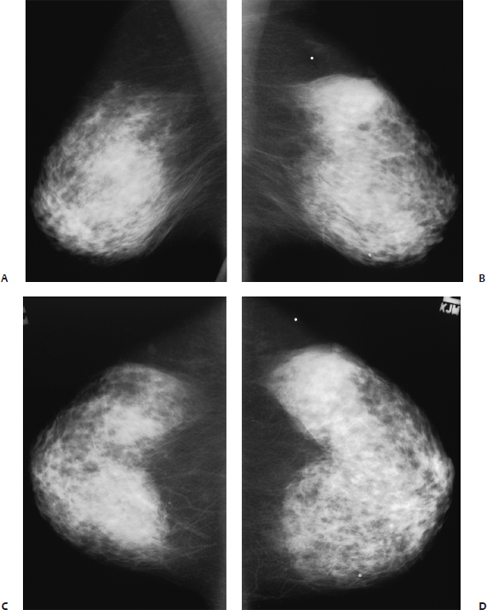
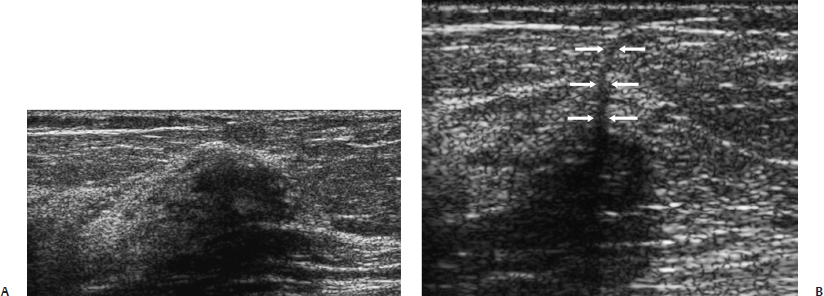
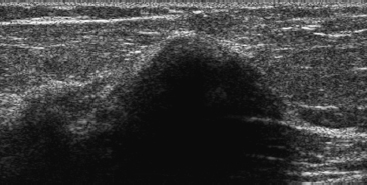
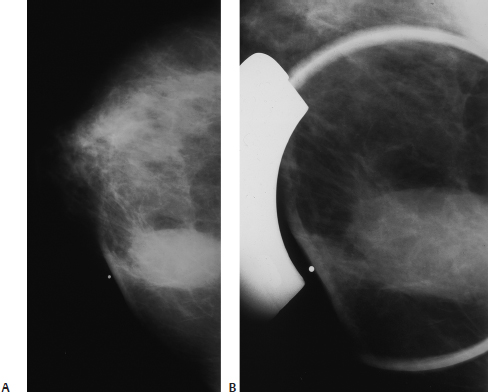
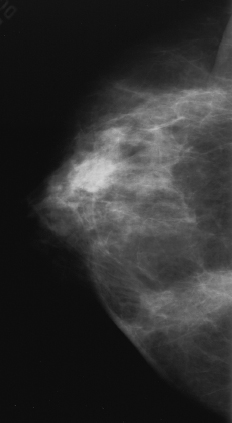
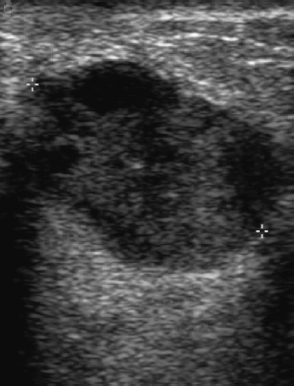
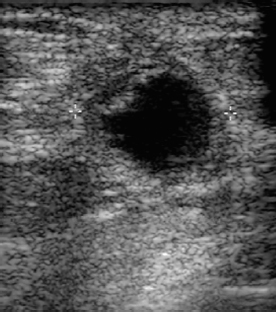
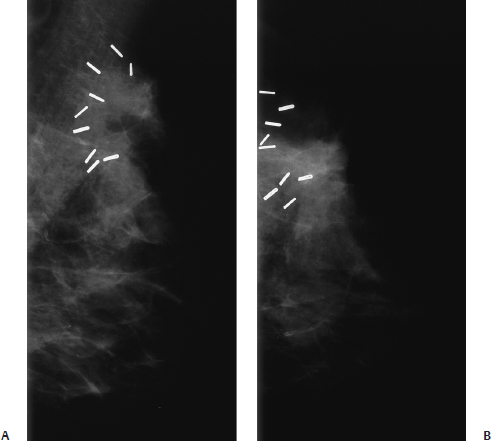
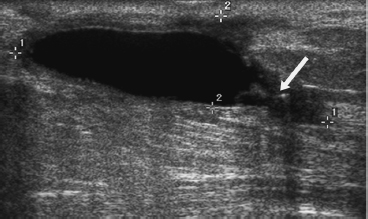
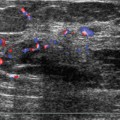
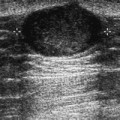
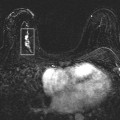
28 After Diagnostic or Therapeutic Procedures for Neoplasm A 77-year-old woman presents for screening right breast mammogram. She had a left mastectomy for neoplasm and a benign right excisional biopsy several years ago. • Normal exam Fig. 28.1 In the right subareolar area, there are disruption and distortion of the ductal system. This architectural distortion resulted from the patient’s benign excisional biopsy and has been stable for at least 10 years. (A) Right MLO mammogram. (B) Right CC mammogram. • Scar • BI-RADS assessment category 2, benign finding • Mammographically, a scar presents as architectural distortion or irregular density. Patients treated for malignancy demonstrate scarring more often than those treated for benign lesions. One year after surgery, more than 90% of patients treated with lumpectomy and radiation therapy have mammographically detectable scars compared with less than 50% for those experiencing benign excisional biopsies. Five years after surgery, architectural distortion is mammographically evident in 70 and 20%, respectively. Brenner RJ, Pfaff JM. Mammographic features after conservation therapy for malignant breast disease: serial findings standardized by regression analysis. AJR Am J Roentgenol 1996;167:171–178 Mendelson EB. Evaluation of the postoperative breast. Radiol Clin North Am 1992;30:107–138 Sickles EA, Herzog KA. Mammography of the postsurgical breast. AJR Am J Roentgenol 1981;136:585–588 A 66-year-old woman had left breast lumpectomy and radiation therapy 6 months ago. • Left breast: large scar; otherwise normal exam • Right breast: normal exam Mass (Fig. 28.2) • Margin: spiculated • Shape: irregular • Density: high Fig. 28.2 In the site of a previous lumpectomy, there are irregular density, architectural distortion, spiculation, skin thickening, and retraction. (A) Left MLO mammogram. (B) Left CC mammogram. • Scar • BI-RADS assessment category 2, benign finding • Within the first year, the density associated with breast excision is a combination of hematoma, fat necrosis, and scar. The combination of these abnormalities will produce either an ill-defined regional density or a focal irregular mass. When the postoperative lesion is a regional density, the density may decrease in size, but it tends to persist even after 5 years. However, when the postsurgical abnormality is a mass, it tends to completely resolve. Brenner RJ, Pfaff JM. Mammographic features after conservation therapy for malignant breast disease: serial findings standardized by regression analysis. AJR Am J Roentgenol 1996;167:171–178 A 77-year-old woman had a right lumpectomy and radiation 2 years ago. • Right breast: lumpectomy scar; otherwise normal exam • Left breast: normal exam Mass (Figs. 28.3 and 28.4) • Margin: spiculated • Shape: irregular • Density: equal density Fig. 28.3 These mammograms were performed 1 year after a lumpectomy and radiation therapy. There is an ill-defined density associated with the clips from the previous lumpectomy. (A) Right MLO mammogram. (B) Right exaggerated CC mammogram. Fig. 28.4 These mammograms were performed 2 years after a lumpectomy and radiation therapy. There has been a subtle increase in the density associated with the surgical clips. (A) Right MLO mammogram. (B) Right CC mammogram. (C) Right CC spot compression mammogram. Low Frequency Frequency • 7 MHz Mass (Fig. 28.5) • Margin: spiculation/architectural distortion • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: severe shadowing, mass completely obscured • Shape: irregular Fig. 28.5 Right breast radial sonogram. With lower frequency sonography, the lumpectomy site still exhibits an irregular, hypoechoic solid mass. Surgical clips (arrows). Frequency • 11.5 MHz (Fig. 28.6) Fig. 28.6 Right breast radial sonogram. With high-frequency sonography, the lumpectomy site is an irregular hypoechoic, heavily shadowing mass. • Scar • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Usually, scars remain unchanged or diminish in mammographic density and size. However, if the mammographic density of an excisional site increases and the site exhibits a sonographic mass, then biopsy is indicated. • Sonographically, scars commonly cause severe posterior acoustic shadowing. If this shadowing is present when using a high frequency, switch to low frequency. A benign scar produces a hyperechoic irregularity without a mass. However, this case illustrates that some scars appear identical to malignancies. Mendelson EB. Imaging the post-surgical breast. Semin Ultrasound CT MR 1989;10:154–170 A 61-year-old woman has had 6 months of left breast pain. She had a benign left breast biopsy 20 years ago. • Left breast: scar in left upper outer quadrant; also extremely tender to palpation in the upper outer quadrant • Right breast: diffusely mildly tender, otherwise normal exam Fig. 28.7 Bilateral normal mammograms. (A) Right MLO mammogram. (B) Left MLO mammogram. (C) Right CC mammogram. (D) Left CC mammogram. Low Frequency Frequency • 10 MHz (Fig. 28.8) Fig. 28.8 With lower frequency in the radial view (A), the scar appears to be a hypoechoic area, but the antiradial view (B) demonstrates that the lesion corresponds to a thin line of architectural distortion associated with shadowing (arrows). (A) Left radial breast sonogram. (B) Left antiradial breast sonogram. High Frequency Frequency • 13 MHz (Fig. 28.9) Fig. 28.9 Left radial breast sonogram. The patient’s scar was in the middle of the area of tenderness. With high frequency, the scar creates severe shadowing, so the benign nature of this lesion is not visible. • Scar • BI-RADS assessment category 2, benign finding • In an area of surgical excision, a scar can be mammographically differentiated from a neoplasm in the following ways: (1) identify lucencies within the center of the scar, (2) observe that the scar changes in appearance with different views, and (3) note decreases in size or density of the lesion on sequential exams. • Sonographically, scars have the following characteristics: (1) scars are hyperechoic, (2) they exhibit different appearances with different angles, and (3) benign scars have no associated hypoechoic mass (which is visible on two views). Because scars strongly attenuate sound, lower-frequency sonography is generally better than higher-frequency sonography in characterizing scars. Mendelson EB. Evaluation of the postoperative breast. Radiol Clin North Am 1992;30:107–138 A 63-year-old woman presents 3 months after right lumpectomy for breast cancer. She now has a lump in her surgical site. • Right breast: tender, palpable lump in the lumpectomy site • Left breast: normal exam Mass (Figs. 28.10 and 28.11) • Margin: circumscribed • Shape: oval • Density: equal density Fig. 28.10 Three months after the patient’s right lumpectomy, there is an ill-defined oval mass associated with the lumpectomy site. The palpable lump corresponds to this mass. (A) Right CC mammogram. (B) Right CC spot compression mammogram. Fig. 28.11 Right CC mammogram. Ten months after the patient’s surgery, the oval mass has decreased in size and density. Frequency • 7 MHz Mass (Figs. 28.12 and 28.13) • Margin: well defined • Echogenicity: heterogeneous (mixed) • Retrotumoral acoustic appearance: increased acoustic transmission • Shape: ellipsoid Fig. 28.12 Right transverse breast sonogram. Three months after surgery, the palpable lump is a sonographically complex, well-defined fluid collection with heterogeneous echo-genicity and increased acoustic transmission. Fig. 28.13 Right transverse breast sonogram. Sonographic examination 10 months after surgery demonstrates that the fluid collection has greatly decreased in size. The fluid is anechoic and surrounded by thick walls. Anterior to the fluid, there is architectural distortion with skin thickening. • Hematoma • BI-RADS assessment category 2, benign finding • Hematomas or seromas have been observed in 50% of patients 1 month after surgery. These lesions tend to resolve, so only 25% of patients exhibit fluid collections 6 months after excision. However, rarely patients will have persistent seromas years later. • Mammographically, the hematoma/seroma typically appears as an oval mass of water density. Sometimes, the mass may demonstrate fat-fluid layering on 90-degree lateral views. The margins may be well defined, ill defined, or spiculated. • Sonographically, the hematoma/seroma is a hypoechoic, anechoic, or heterogeneous fluid collection. Internal septations and dependent solid material may be present. Soo MS, Williford ME. Seromas in the breast: imaging findings. Crit Rev Diagn Imaging 1995;36:385–440 A 59-year-old woman had excision of ductal carcinoma in situ (DCIS) and radiation therapy 4 months ago. She now notes a ridge next to her lumpectomy site. • Left breast: vague ridge of tissue in the axilla near healing scar • Right breast: normal exam • Asymmetric density (Fig. 28.14) Fig. 28.14 In the left upper outer breast, there are clips and ill-defined density in the lumpectomy site. (A) Left MLO mammogram. (B) Left exaggerated CC mammogram. Frequency • 14 MHz Mass (Figs. 28.15 and 28.16) • Margin: ill defined • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: single edge shadowing • Shape: irregular
Case 28.1: Scar—Architectural Distortion
Case History
Physical Examination
Mammogram (Fig. 28.1)
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 28.2: Scar—Architectural Distortion
Case History
Physical Examination
Mammogram
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 28.3: Scar—Irregular Density
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 28.4: Scar—Sonographic Technique
Case History
Physical Examination
Mammogram (Fig. 28.7)
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 28.5: Hematoma
Case History
Physical Examination
Mammogram
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 28.6: Fat Necrosis
Case History
Physical Examination
Mammogram
Ultrasound
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree