CMS sets reimbursement rates for medical services provided, including technical and professional fees for imaging studies. Furthermore, CMS’s fee schedules often affect reimbursement rates for local private insurance carriers. CMS requirements also dictate requirements for providers and facilities. For example, CMS requires that all outpatient facilities that bill CMS for the technical component for advanced imaging studies (CT, MRI, and PET) be accredited by an organization with deeming authority.1
Centers for Disease Control and Prevention
The Centers for Disease Control and Prevention (CDC) is a large agency of the DHHS. The CDC is charged with detecting and responding to new and emerging health threats; confronting the biggest health problems that cause death and disability for Americans; using science and advanced technology to prevent disease; promoting health and safe behaviors, communities, and environments; developing leaders and training the public health workforce; and assessing the health status of the United States.2
The CDC provides educational materials for providers and the public on specific diseases, healthy lifestyles, travel risks and recommendations, emergency preparedness, and other public health topics. Furthermore, through the National Center for Health Statistics, the CDC provides a wealth of public health data.
The National Institute for Occupational Safety and Health (NIOSH) is a unit of the CDC that conducts research and makes recommendations to prevent worker injury and illness. NIOSH runs the B Reader Program, which began in 1974 in response to the need to identify physicians qualified to serve in national pneumoconiosis programs directed at coal miners.3 The Federal Mine Safety and Health Act of 1977 mandated the creation of the Coal Workers’ X-ray Surveillance Program, which requires B reader certification for interpreters of worker radiographs. B reader certification is also required for the Asbestos Medical Surveillance Program, which is administered by the Navy and Marine Corps Public Health Center.
Food and Drug Administration
The Food and Drug Administration (FDA) is an agency in the DHHS and is responsible for protecting public health by assuring the safety of the food supply (certain animal products such as meat are regulated by the US Department of Agriculture); ensuring that human and veterinary drugs, vaccines, and other biologic products and medical devices for human use are safe and effective; protecting the public from electronic product radiation; assuring cosmetics and dietary supplements are safe and properly labeled; regulating tobacco products; and advancing public health by helping speed product innovations.4 For example, CT and MRI scanners, contrast agents, intravascular catheters, and computer-aided detection (CAD) software all must receive FDA clearance before being routinely implemented in health-care delivery. The FDA also administers the Mammography Quality Standards Act (MQSA) (see Chapter 8).
State Medical Boards
All the 50 US states, the District of Columbia, and US territories have laws that regulate the practice of medicine and define the responsibility of the state or territorial medical board. Depending on state or territorial law, medical boards are either independent agencies or part of a larger umbrella such a state health department. There are currently 70 medical and osteopathic medical boards in the United States and its territories, which are represented by the not-for-profit Federation of State Medical Boards (FSMB).
State medical boards grant licenses for the general practice of medicine and do not limit practice to specific medical specialties. Furthermore, physicians are not required to hold board certification in a medical specialty to be granted a license. Requirements for licensure, including postgraduate training requirements, number of attempts at licensing examination (United States Medical Licensing Examination), and time limit for completing licensure examination sequence, vary by jurisdiction. In some jurisdictions, licenses for other health-care practitioners such as physician assistants, physical therapists, and acupuncturists are issued by state medical boards.
State medical boards are also responsible for investigating complaints against practitioners, disciplining practitioners who violate state laws, and evaluating and facilitating rehabilitation for impaired physicians.5
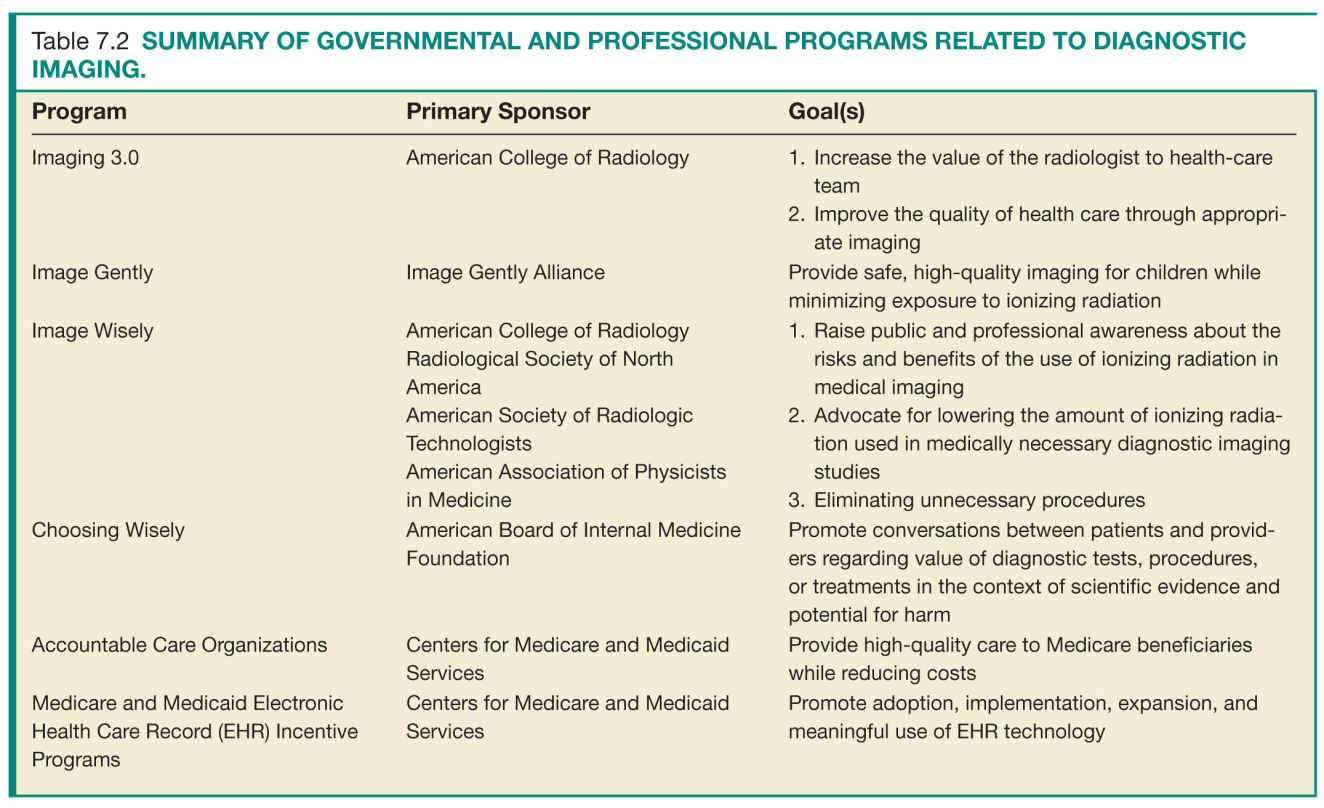
PROGRAMS
Imaging 3.0
Imaging 3.0 is a campaign developed and promoted by the American College of Radiology (ACR), with the strategic goals of preserving radiologist relevance while improving patient care in the era of US health-care reform.6 For patients, Imaging 3.0 focuses on providing better care at lower cost, improving population health, and empowering patients to make informed decisions regarding their own personal health care. For radiologists, Imaging 3.0 promotes practice patterns that increase radiologist relevance, develops tools that enhance the value of radiologists to all stakeholders, and seeks alternatives to continued reduction in fee-for-service (FFS) payments. One of the main thrusts of Imaging 3.0 is the role of the radiologist beyond image interpretation. The ACR seeks to redefine the radiologist’s role to one that begins when imaging is considered and does not end until both the patient and referring physician fully understand the results of the imaging test and any recommendations based on the findings of the imaging study.
Coordinating Care
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree