Allergic Bronchopulmonary Aspergillosis
Gerald F. Abbott, MD
Key Facts
Terminology
Chronic airway inflammation and injury from colonization and sensitization by Aspergillus fumigatus and related species
Imaging Findings
Central bronchiectasis and mucoid impaction in asthmatic patient
Mucoid impaction may have higher attenuation than soft tissue in 30%
Migratory fleeting pulmonary opacities may be seen early, before development of bronchiectasis
Bronchiectasis in 3 or more lobes in asthmatics highly suggestive of ABPA
Confident diagnosis of ABPA in 90% of patients with eosinophilic lung disease
Top Differential Diagnoses
Cystic Fibrosis
Asthma
Congenital Bronchial Atresia
Pathology
1-2% of asthmatic patients have ABPA
10% of patients with cystic fibrosis have ABPA
Clinical Issues
Recurrent ABPA may result in widespread bronchiectasis and fibrosis
Oral corticosteroids treatment of choice
Serial measurement of serum IgE useful to monitor response to therapy
ABPA may recur in patients with cystic fibrosis who have had lung transplantation
TERMINOLOGY
Abbreviations and Synonyms
Allergic bronchopulmonary aspergillosis (ABPA)
Definitions
Chronic airway inflammation and injury from colonization and sensitization by Aspergillus fumigatus and related species
Hypersensitivity reaction that occurs almost exclusively in patients with asthma and cystic fibrosis
IMAGING FINDINGS
General Features
Best diagnostic clue: Central bronchiectasis and mucoid impaction in asthmatic patient
Patient position/location
Central bronchiectasis (may spare peripheral airways)
Predominantly upper lobes
CT Findings
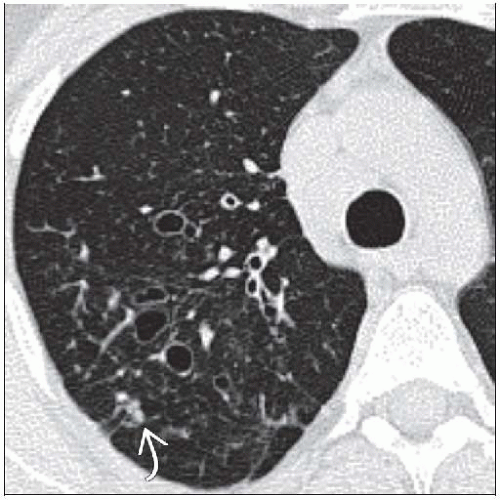
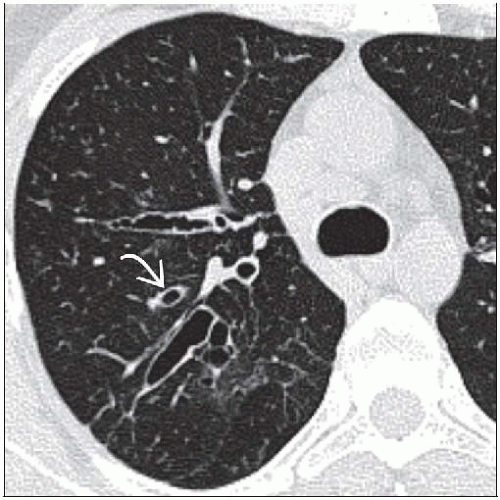
Bronchiectasis (95%)
Bronchiectasis ranges from cylindrical (early) to saccular (advanced)
May be air-filled or filled with soft tissue (mucoid impaction)
Y- or V-shaped tubular opacities emanating from hilum
Mucoid impaction (70%)
Homogeneous tubular &/or branching “finger-in-glove” opacities
Mucoid impaction may have higher attenuation than soft tissue (30%)
Centrilobular nodules, tree-in-bud opacities in distal lung (90%)
May contain air-fluid levels
Distal lung (curiously) usually remains aerated rather than collapsed
Eosinophilic pneumonia
Migratory fleeting pulmonary opacities may be seen early, before development of bronchiectasis
Associated findings
Areas of consolidation, ground-glass opacity due to pneumonia or atelectasis distal to airway obstruction
Pleural effusions absent
Lymphadenopathy, mild in 5%
Location
Zonal distribution of bronchiectasis
Upper lobes (50%)
Lower lobes (20%)
Random (30%)
Axial distribution of bronchiectasis
Central (60%)
Random (30%)
Peripheral (10%)
Mainly involves segmental and subsegmental bronchi
Bronchiectasis in 3 or more lobes in asthmatics highly suggestive of ABPA
Observer accuracy
Confident diagnosis of ABPA in 90% of patients with eosinophilic lung disease
Radiographic Findings
Radiography: May be normal
Imaging Recommendations
Best imaging tool: CT much more sensitive for bronchiectasis
DIFFERENTIAL DIAGNOSIS
Cystic Fibrosis
ABPA seen in 10% of patients with cystic fibrosis
Usually younger
Positive sweat chloride skin test
Distribution of bronchiectasis identical
Asthma
Mucoid impaction may be seen in absence of ABPA
Mild cylindrical bronchiectasis may also be seen in asthma alone
ABPA needs to be excluded
Endobronchial Neoplasm
Mucoid impaction usually seen only with slow-growing tumors
Carcinoid or benign tumors such as hamartomas
Usually unilateral in single lobar or segmental distribution
Congenital Bronchial Atresia
Likely sequela of vascular insult to lung during early fetal development
Thin membranous point of atresia; normal airway distal to atresia
Segmental bronchus does not communicate with central airway
Mucocele develops distal to point of obstruction; round, ovoid, or tubular opacity that may be branching
Often misdiagnosed as arteriovenous malformation
Apical posterior segment of left upper lobe most common but may occur in any part of lung
Difficult to distinguish from ABPA
Look for
Wedge-shaped area of hyperinflation of lung with decreased vascular markings surrounding mucocele
No history of allergies or cystic fibrosis
Primary Ciliary Dyskinesia
Characterized by immotile or dyskinetic cilia; leads to poor mucociliary clearing and development of bronchiectasis
Other manifestations include hearing loss and male infertility
Dextrocardia in patients with Kartagener syndrome
Airway Obstruction from Foreign Body
Look for radiopaque foreign body or broncholith
Unilateral distribution in single segment or lobe
Bronchocentric Granulomatosis
Rare hypersensitivity lung disease may be caused by Aspergillus species
Can be seen with ABPA or separate from it as response to infection with Mycobacterium, other fungi, or Echinococcus
Distal airway lumen replacement by necrotizing granulomas
Imaging similar to ABPA, may predominantly affect more distal airway
Can have focal mass or lobar consolidation with atelectasis
Williams-Campbell Syndrome
Rare congenital deficiency of cartilage in subsegmental bronchi
Bronchiectasis limited to 4th, 5th, and 6th generation bronchi
PATHOLOGY
General Features
Genetics: Higher frequencies of specific HLA-DR2 and HLA-DR5 genotypes found in association with ABPA
Etiology
Aspergillus fumigatus
Ubiquitous soil fungi
Type 1 hypersensitivity reaction with IgE and IgG release
Other fungi also implicated
Other Aspergillus species or Candida
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree