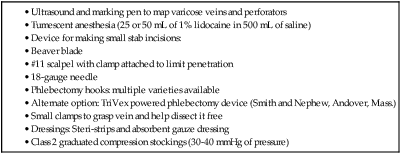
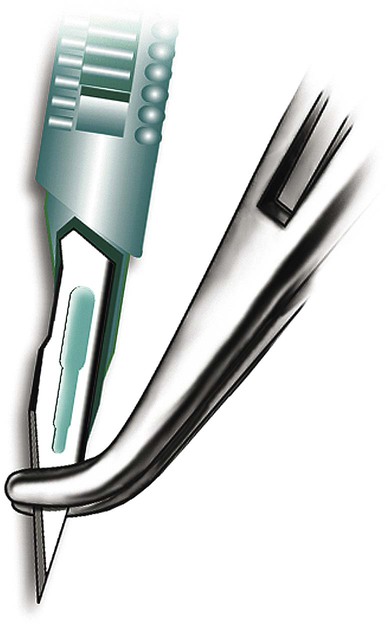
There are some reasons to do AP as primary therapy for varicose veins rather than an adjunct to GSV ablation. Local therapy may be preferable when the deep system is compromised and GSV ablation is inadvisable, or if the varicose veins are fed by a focal source of reflux like a perforating vein. In the latter case, doing GSV ablation without addressing the perforator reflux would lead to clinical failure. This is a more common scenario in patients with more severe venous disease, since it has been shown that there is increasing frequency of refluxing perforators as the clinical severity of venous disease increases.1,2 AP may also be used as palliative treatment to treat local symptoms in a patient who refuses or is medically unable to undergo definitive treatment of the underlying source of reflux. There are very few absolute contraindications to AP. Cellulitis in the planned operative field is a firm contraindication. Operating in an infected field may worsen the infection, and poor healing of the AP incisions is likely. The multidisciplinary guidelines on use of AP also list severe peripheral edema, lymphedema, serious illness, inability to follow postoperative instructions, and allergies to local anesthetics as other absolute contraindications.3 Allergies to local anesthetics may be a contraindication, but switching to a different family of local anesthetics (an ester vs. an amide) can allow safe anesthetic use. Coagulopathy, anticoagulation use, or any other bleeding diatheses are relative contraindications. These abnormalities may increase the risk of bleeding or hematoma. Although these are normally minor complications, greater attention has to be paid to this when doing AP for cosmetic reasons. Even relatively small hematomas or bruising may lead to decreased patient satisfaction if their goal is to improve the cosmetic appearance of the legs. Prior history of deep venous thrombosis is also a relative contraindication, since removal of additional veins may further compromise venous return from the leg. Past episodes of superficial phlebitis or prior attempts at sclerotherapy may not be actual contraindications, but can greatly increase the difficulty of AP if veins are adherent to surrounding tissue. These veins should be approached more cautiously. Table 105-1 offers a list of necessary equipment for performing the AP procedure. TABLE 105-1 The initial step is to map the varicose veins to be treated. This is done before the procedure, with the patient standing to distend the veins. The skin over the varices to be removed should be marked on with a marker. If this is not done, the varices may not be visible when the patient is supine (Fig. 105-1). The tumescent anesthetic solution is formulated by diluting either 25 or 50 mL of 1% lidocaine in 500 mL of saline. This yields 0.05% or 0.1% lidocaine, respectively. To reduce the discomfort of the lidocaine injection, the solution should be buffered by adding 5 mL of 8.4% sodium bicarbonate. It is recommended that the total volume of anesthetic used be limited to 5 mg of lidocaine per kilogram of body weight.3 Lidocaine with epinephrine can be used to reduce bleeding, but bleeding is rarely severe enough to require it, and skin necrosis has been attributed to epinephrine use in one case report.4 For best cosmetic results, incisions should be very small, approximately 1 to 2 mm in length. These small incisions do not require sutures, which facilitates healing without significant scarring. A #11 scalpel blade can be used to make the stab incisions, but care must be taken to avoid advancing the blade in too far, which would lead to a larger incision by virtue of the blade’s triangular shape. Placing a clamp on the blade can help limit the depth of penetration (Fig. 105-2). Small stab incisions can also be made with an 18-gauge needle. A Beaver blade (Fig. 105-3) is ideal for phlebectomy; it is a microblade that by virtue of its small size will limit the size of the incision.
Ambulatory Phlebectomy
Indications
Contraindications
Equipment
Technique

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine







