Presentation and Presenting Images
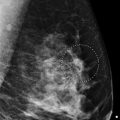
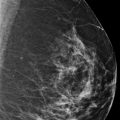
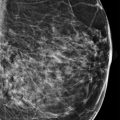
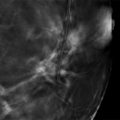
A 47-year-old female presents for screening mammography.
29.2 Key Images
29.2.1 Breast Tissue Density
The breasts are extremely dense, which lowers the sensitivity of mammography.
29.2.2 Imaging Findings
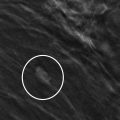
In the upper outer quadrant of the right breast at the 10 o’clock location in the anterior depth, there are grouped calcifications. These are very hard to discern on the digital breast tomosynthesis (DBT) images.
29.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
29.4 Diagnostic Images
( ▶ Fig. 29.5, ▶ Fig. 29.6, ▶ Fig. 29.7, ▶ Fig. 29.8, ▶ Fig. 29.9, ▶ Fig. 29.10, ▶ Fig. 29.11, ▶ Fig. 29.12, ▶ Fig. 29.13)
29.4.1 Imaging Findings
The diagnostic imaging demonstrates a 2.5-cm area of segmental amorphous calcifications in the right breast at the 10 o’clock location, 1.5 cm from the nipple. The calcifications do not layer. The morphology of these calcifications warrant a biopsy. The patient reports that she had a biopsy about 6 years ago. These records were located including the stereotactic biopsy images ( ▶ Fig. 29.9, ▶ Fig. 29.10, and ▶ Fig. 29.11). The specimens from the stereotactic biopsy contain numerous calcifications, which indicate that the area was well-sampled. No biopsy clip was placed according to the procedure report due to bleeding. Comparing the current imaging and the imaging 2 years after the biopsy ( ▶ Fig. 29.12 and ▶ Fig. 29.13), these calcifications are stable. The biopsy diagnosis 6 years ago was sclerosing adenosis.
29.5 BI-RADS Classification and Action
Category 2: Benign
29.6 Differential Diagnosis
Sclerosing adenosis: These calcifications when biopsied revealed sclerosing adenosis. Overall the calcifications are stable with no increase compared to prior examinations. Amorphous calcifications are consistent with sclerosing adenosis.
Ductal carcinoma in situ (DCIS): DCIS would be a concordant biopsy result for amorphous calcifications. The fact that these calcifications have been stable and have a benign concordant biopsy result makes DCIS less likely in this case, but it was a concern at initial presentation.
Fibrocystic disease: Fibrocystic changes can present with various underlying mammographic findings such as cysts, masses, and calcifications. When calcifications are present, these can be seen to layer in cysts, but atypical presentations can occur and thus there is a significant overlap of fibrocystic changes and ADH (atypical ductal hyperplasia) and/or DCIS on the biopsy of grouped calcifications.
29.7 Essential Facts
Sclerosing adenosis commonly presents as grouped and/or scattered amorphous calcifications. It is often indistinguishable from low-grade DCIS. Biopsy is frequently performed to exclude DCIS.
Sclerosing adenosis can present mammographically as a mass, an architectural distortion, and calcifications.
Sclerosing adenosis has many overlapping imaging findings with both invasive and intraductal cancer.
Sclerosing adenosis is a benign proliferative breast disease.
In addition to DBT not performing as well in identifying the distribution of calcifications, the low-dose radiation of DBT produces a much noisier projection view compared to full-field digital mammography (FFDM), which has both negative qualitative and quantitative effects on the analysis of calcifications on DBT. This is especially true for those amorphous, or finer,, calcifications.
29.8 Management and Digital Breast Tomosynthesis Principles
Prior imaging studies, especially when accessible, can avert unnecessary biopsies or additional imaging.
Sclerosing adenosis can exist in the midst of other significant pathology. When assessing the concordance of radiology and pathology, it is important to assess if the imaging findings correlate with the pathology findings. If the lesion is large and only a microscopic area of a certain pathology is found, it is unlikely that the pathology explains the imaging findings. If there is doubt, it is often helpful to discuss or review the slides with the pathologist if this is not a routine practice in a radiology–pathology concordance program.
When patients have had prior biopsies and no biopsy markers are placed, it is important to correlate prior imaging, procedure information, and medical records to the current mammography and other imaging findings to ensure that the proper management is performed.
29.9 Further Reading
[1] Gill HK, Ioffe OB, Berg WA. When is a diagnosis of sclerosing adenosis acceptable at core biopsy? Radiology. 2003; 228(1): 50‐57 PubMed
[2] Uematsu T. The emerging role of breast tomosynthesis. Breast Cancer. 2013; 20(3): 204‐212 PubMed

Fig. 29.1 Right craniocaudal (RCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree