Anatomy and Embryology
▪ ANATOMY
Adrenal Gland
The adrenal glands share the perinephric space with the kidneys. The right adrenal lies above and anteromedial to the upper pole of the right kidney and is best seen on axial imaging immediately posterior to the inferior vena cava (IVC) just below the liver. The left adrenal is also anteromedial to the ipsilateral kidney, is usually seen at about the same level as the upper renal pole, and lies posterior to the pancreas. The right adrenal typically has an inverted Y appearance, whereas the left tends to resemble a threepointed star (Fig. 1.1). In patients with renal agenesis or ectopy, the ipsilateral adrenal gland has a linear shape (Fig. 1.2). Each gland weighs approximately 5 g, and each limb typically varies from 3 to 6 mm in width, though up to 1 cm may be considered normal. The small size makes it difficult to distinguish a normal from an atrophic or hyperplastic adrenal gland on the basis of size alone.
The arterial supply to the adrenal glands consists of many small branches from three main feeding arteries, producing a comblike appearance (Fig. 1.3). The superior adrenal artery, usually a branch from the inferior phrenic artery, supplies the superior portion of the gland. The middle adrenal artery, arising directly from the aorta, provides vessels to the midportion. The inferior gland is fed by branches from the inferior adrenal artery, which most often arises from the ipsilateral renal artery.
Each adrenal gland is drained by a single central vein. On the right, the adrenal vein enters directly into the posterior aspect of the IVC (Fig. 1.4). Occasionally, however, the adrenal vein may join an accessory hepatic vein before entering the IVC. The left adrenal vein enters the inferior phrenic vein before joining the left renal vein. The right adrenal vein is shorter and has a smaller diameter than the left, so it is more difficult to obtain a venous sample from the right adrenal vein than from the left.
Urinary Tract
Kidneys
The kidneys are paired, retroperitoneal structures that parallel the psoas muscle on either side of the lumbar spine. The left kidney is usually slightly more superior than the right kidney. The long axes of the kidneys are deviated approximately 20° from the spine, with the top of the kidneys closer to the spine. There is often considerable motility of each kidney, which varies with respiration and with body position; several centimeters of excursion may be demonstrated on deep inspiration or in the upright position.
The kidney is composed of a variable number of renal pyramids. Each pyramid consists of a minor calyx and its associated ducts. The base of the pyramid is formed by its overlying renal cortex, and its apex is formed by the renal papilla, which projects into a minor calyx. The papillae are cone-shaped structures that contain the openings of the distal collecting ducts (of Bellini), which empty into the calyces. A calyx is a cup-shaped portion of the intrarenal collecting system. The rim of the cup is called the fornix. Several papillae may project into a single larger calyx, which is then called a compound calyx. Urine drains from each calyx into an infundibulum; each infundibulum may either drain directly into the renal pelvis or join other infundibula to form a larger conduit (sometimes called a major infundibulum) that then empties into the pelvis. The pelvis may rest primarily in the renal sinus or project through the renal hilus; if it is primaily outside the hilus, it is sometimes called an extrarenal pelvis and is normally more voluminous than a typical intrarenal pelvis.
The kidney may be divided into an outer cortex and an inner medulla. The arcuate artery at the base of each pyramid marks the junction between the cortex and the medulla. Columns of cortical tissue, however, may descend between the medullary pyramids. These columns have been termed the septal cortex, but they are more commonly referred to as columns of Bertin (or Bertini). The calyces, the infundibula, and the renal pelvis are jointly referred to as the “intrarenal collecting system.” The renal sinus, or central
cavity of the kidney, contains the collecting system and a variable amount of fat.
cavity of the kidney, contains the collecting system and a variable amount of fat.
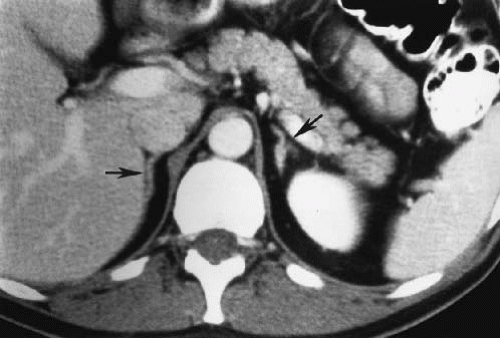 FIGURE 1.1. Normal adrenal glands. The right adrenal (arrow) lies behind the IVC and medial to the liver. The left adrenal (arrow) is anteromedial to the upper pole of the left kidney. |
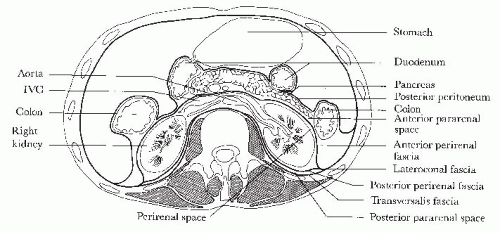
The kidneys are loosely enclosed in an envelope of perirenal fascia known as “Gerota fascia” (Fig. 1.5). The retroperitoneum is defined by various fascial layers and is divided into three discrete compartments: the anterior pararenal space, the perirenal space, and the posterior pararenal space.
The anterior pararenal space extends from the posterior portion of the peritoneal cavity to the anterior layer of Gerota fascia. The anterior pararenal space contains the pancreas, the second through fourth portions of the duodenum, the ascending and descending colon, and the hepatic and splenic arteries.
The perirenal space is defined by the anterior and posterior layers of Gerota fascia. The two layers of perirenal fascia may be fused in the midline or the anterior and posterior leaves may continue across the midline without fusing, allowing free communication between the two perirenal spaces. The anterior and posterior layers of the perirenal fascia form an envelope, which contains the kidney, adrenal gland, and proximal ureter, and finally merge into the lateroconal fascia laterally. The perinephric space, when viewed three-dimensionally, is cone shaped and filled with the kidney and perinephric fat. It is still debated as to whether this cone-shaped perinephric space is open or closed inferiorly and therefore whether it communicates with the pelvic extraperitoneal space.
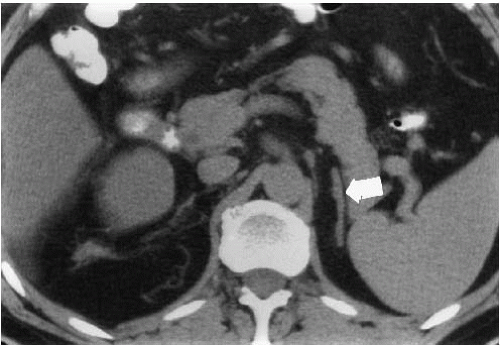 FIGURE 1.2. Left renal agenesis. The left adrenal gland (arrow) has a linear appearance rather than showing the typical three limbs. |
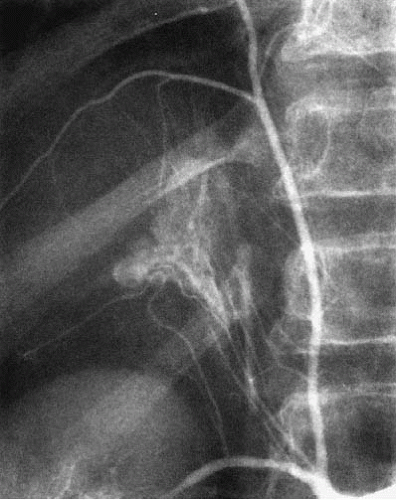 FIGURE 1.3. Adrenal arteries. The adrenal gland is supplied by many small arterial branches that arise from the inferior phrenic artery, aorta, and renal artery. |
The posterior pararenal space is defined anteriorly by the posterior layer of the perirenal fascia and posteriorly by the fascia that covers the psoas and quadratus lumborum muscles. The posterior pararenal space contains no organs.
Unlike the retroperitoneum, the pelvic extraperitoneal space is not truly anatomically divided; however, it is often divided into four potential spaces for descriptive purposes: (1) the space of Retzius (the anterior extraperitoneal space) between the symphysis pubis and the bladder, (2) the retrovesical space between the bladder and the rectum, (3) the presacral space between the rectum and the sacrum, and (4) the perirectal space that surrounds the rectum.
The function and vascular anatomy of the kidney are discussed in subsequent chapters.
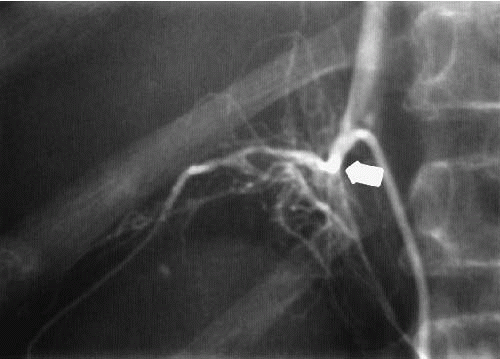 FIGURE 1.4. Adrenal vein. A single draining right adrenal vein (arrow) enters directly into the IVC. |
Ureters
The ureter is a muscular conduit that transports urine from the renal pelvis to the bladder (Fig. 1.6). It begins at the ureteropelvic junction, which is usually a gentle tapering of the renal pelvis as it joins the ureter. The ureter remains retroperitoneal throughout its course, crossing the psoas muscle obliquely from lateral to medial. It crosses anterior to the common or external iliac artery and then courses posteroinferiorly as it enters the pelvis, where it curves laterally and then medially before entering the posterolateral aspect of the bladder floor at the ureterovesical junction. The ureters enter the bladder obliquely and course submucosally for about 2 cm before terminating at the lateral margin of the trigone as the ureteral orifice. The ureterovesical junction is the narrowest portion of the ureter.
 FIGURE 1.6. Normal course of the ureters. Note the smooth lateral curve of the ureters in the pelvis before entering the bladder. |
The ureter is composed of mucosal, muscular, and adventitial layers. The mucosa is covered by transitional epithelium that is continuous with that of the renal pelvis proximally and the bladder distally. When the ureter is empty, the mucosa collapses into longitudinal folds.
The muscular layer has both circular and longitudinal muscle fibers separated by fibroareolar connective tissue. In the distal ureter, longitudinal muscle fibers continue in the intravesical portion of the ureter and decussate with muscles of the trigone.
The ureter receives its arterial supply from many sources. The renal arteries provide branches to the renal pelvis and proximal ureter. The aorta and lumbar, gonadal, and iliac arteries supply the midportion of the ureter. The predominant vessel supplying the distal ureter is the inferior vesical artery. In females, the uterine artery often sends branches to the ureter.
Urine is moved from the kidney to the bladder primarily by peristalsis. Contractions begin in the collecting system and propel urine into the pelvis. Each contraction begins as a response to the stretching of the pelvic wall, which is caused as the kidney continuously produces urine. Diuresis stretches the wall more rapidly and results in more frequent contraction waves.
Each bolus of urine is propelled down the ureter by smoothly successive relaxations and contractions of smooth muscle fibers propagated by nexi connecting the muscle fibers. The ureter is an aganglionic organ, and therefore peristalsis is not related to neural activity. During peristalsis, pressures of 20 to 35 mm Hg are sufficient to propel a bolus of urine from the ureter into the resting bladder.
Bladder
The bladder is a hollow pelvic viscus consisting of smooth muscle, lamina propria, submucosa, and mucosa. The muscle is the detrusor muscle, which consists of three layers: an inner longitudinal, a middle circular, and an outer longitudinal. Each layer is closely applied to the other without separating laminae or fasciae. The three muscle layers condense inferiorly to form the trigone, a muscular triangle with the apex extending to the bladder neck. The ureters enter the bladder at the lateral aspects of the trigone. Between the ureteric orifices is a muscular ridge, known as the interureteric ridge, which forms the base of the trigone. Outer longitudinal detrusor muscle fibers extend inferiorly to the bladder base and may contribute to the opening of the bladder neck when the detrusor
muscle contracts during voiding. The internal sphincter, a separate circular smooth muscle sphincter, is located at the bladder neck.
muscle contracts during voiding. The internal sphincter, a separate circular smooth muscle sphincter, is located at the bladder neck.
The adult bladder lies deep in the pelvis when empty, but the flexibility of the detrusor muscle fibers allows the bladder walls and dome to rise high in the pelvis when the bladder is full. The bladder is extraperitoneal, but its dome and the upper third of its lateral walls are loosely covered by the peritoneum. When the bladder is empty, the peritoneum extends deep into the pelvis; when the bladder is full, the peritoneum is elevated. The male bladder is adjacent to the rectum posteriorly, the ampulla of the vas deferens and seminal vesicles posteroinferiorly, and the prostate base inferiorly. In females, the uterine fundus is usually anteflexed over the bladder dome, whereas the cervix and vagina lie posterior to the bladder.
Arterial supply to the bladder is through superior, middle, and inferior vesical arteries arising from the hypogastric arteries. Additional arterial blood may come from branches of the obturator artery, the vas deferens artery, and the inferior gluteal artery. In females, additional branches from the uterine and vaginal arteries may supply the lateral and inferior bladder walls. Capillaries from these arteries form a rich arterial network around the bladder. Consequently, there is a rich vesical venous plexus that surrounds the bladder and flows directly into the hypogastric (internal iliac) veins. Auxiliary veins connect the vesical venous plexus to the hemorrhoidal veins that drain into the intervertebral venous plexus. This is the route of vesical venous drainage when the IVC is blocked. In addition, a rich network of vesical lymphatics drains into the internal and external iliac nodes, with continued drainage into the common iliac and paraaortic nodes.
The innervation of the bladder, as well as the physiology of bladder emptying, is discussed in Chapter 15 in the section on neurogenic bladder.
Male Urethra
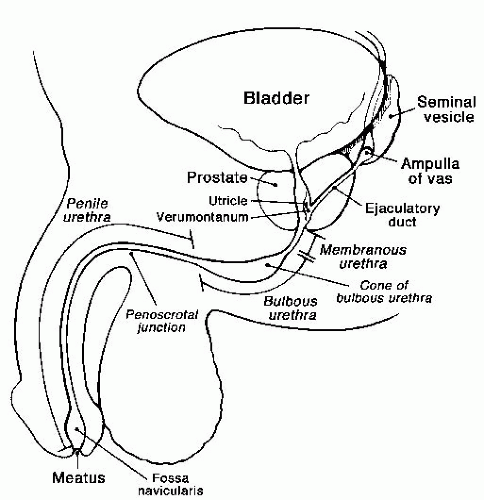
The male urethra consists of posterior and anterior portions, each of which is subdivided into two parts (Fig. 1.7).
Posterior Urethra
The posterior urethra extends from the bladder neck to the inferior aspect of the urogenital diaphragm and is divided into prostatic and membranous portions. The prostatic urethra is approximately 3.5 cm in length, passes through the prostate gland, and ends at the superior aspect of the urogenital diaphragm. A longitudinal ridge of smooth muscle extends from the bladder neck to the membranous urethra on the posterior wall of the posterior urethra. This longitudinal smooth muscle bundle swells just proximal to the membranous urethra to form a 1-cm-long ovoid mound on the urethral floor, the verumontanum (colliculus). A small depression in the verumontanum is known as the utricle. The ejaculatory ducts empty side by side into the urethra at the distal verumontanum. Above the verumontanum, small submucosal prostatic glands constitute the transitional zone of the prostate. It is in this zone that prostatic hypertrophy, or benign prostatic hyperplasia (BPH), occurs. Consequently, the prostatic urethra may be compressed by prostatic adenomata that may enlarge to obstruct the bladder neck and even indent the bladder base. Rarely do prostatic adenomata extend below the verumontanum. The glands of the transitional zone empty into the floor of the prostatic urethra through approximately 30 to 40 small ostia surrounding the verumontanum. The prostatic urethral mucosa is continuous with the bladder mucosa and is composed of transitional cells, but changes to stratified columnar epithelium at the membranous urethra.
The membranous urethra is the short segment (approximately 1 cm in length) passing through the urogenital diaphragm. This is the narrowest part of the urethra, making it very important to know the anatomical landmarks of the membranous urethra on both antegrade and retrograde urethrography so that it is not mistaken for a stricture. The proximal landmark for the membranous urethra is the distal end of the verumontanum, and the distal landmark is the tip of the cone of the bulbous urethra (Fig. 1.7).
Anterior Urethra
The anterior urethra extends from the inferior side of the urogenital diaphragm to the external urethral meatus. The bulbous urethra begins at the inferior aspect of the urogenital diaphragm and extends to the angulated penoscrotal junction; this is the widest and most inferior portion of the urethra. The proximal bulbous urethra has a conical shape, with a narrow tip as the urethra exits the urogenital diaphragm. The penile (or pendulous) urethra extends from the penoscrotal junction to the meatus. The distal 2 cm of the penile urethra is slightly dilated and known as the fossa navicularis. The anterior urethra is lined by stratified columnar epithelium except at the external meatus, where it changes to stratified squamous epithelium, which extends through the meatus and covers the glans penis.
Periurethral structures will occasionally opacify during urethrography (Fig. 1.8). Along the length of the anterior urethra are small, mucus-secreting submucosal glands, the glands of Littre. These glands, which are numerous in the bulbous urethra and in the superior aspect of the penile urethra, secrete mucus into the urethra during sexual stimulation. The two ducts draining Cowper glands empty into the proximal to midbulbous urethra. These ducts have a very small diameter, are approximately 2 cm long, and drain the glands of Cowper, which lie on either side of the membranous urethra and between the leaves of the urogenital diaphragm. Cowper glands also secrete mucus during sexual stimulation.
The bulbocavernous muscle surrounds the anterior urethra and is involved in emptying the anterior urethra at the end of micturition. A small, striated musculotendinous sling of the bulbocavernous muscle extends from the anterior and lateral surfaces of the proximal bulbous urethra. This structure is known as the musculus compressor nuda (Fig. 1.9) and may circumferentially indent the
proximal bulbous urethra on dynamic retrograde urethrography. This finding, sometimes called “Cobb’s collar,” should not be mistaken for a true stricture.
proximal bulbous urethra on dynamic retrograde urethrography. This finding, sometimes called “Cobb’s collar,” should not be mistaken for a true stricture.
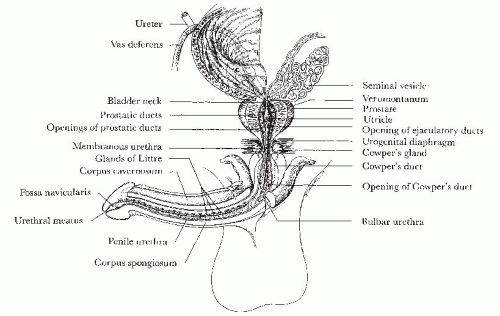 FIGURE 1.8. Male urethra and periurethral structures. (From Amis ES Jr, Newhouse JH, Cronan JJ. Radiology of male periurethral structures. AJR Am J Roentgenol. 1988;151:321-324, with permission.) |
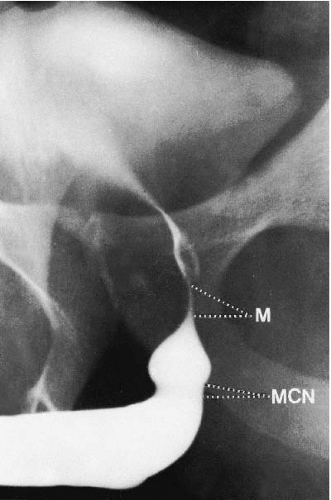 FIGURE 1.9. Dynamic retrograde urethrogram. M, membranous urethra; MCN, musculus compressor nuda. (From McCallum R. The adult male urethra. Radiol Clin North Am. 1979;27:227-244, with permission.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|