26 Anatomy and Normal Doppler Signatures of Abdominal Vessels
Celiac Artery
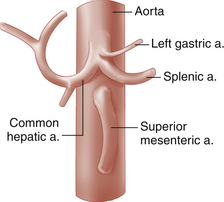
The celiac artery, also called the celiac trunk or celiac axis, is the first major visceral branch of the abdominal aorta. It arises from the anterior aortic surface, between the diaphragmatic crura (Figure 26-1). It then bifurcates about 1 to 3 cm from its origin into the common hepatic and splenic arteries, which are readily visualized with ultrasound. The celiac artery also gives rise to the left gastric artery, which is generally not visible sonographically. The branching pattern of the celiac artery is quite constant, occurring in approximately 93% of individuals. In the most common variations, one or more of the celiac branches arises separately from the aorta or from the superior mesenteric artery (SMA). In less than 1% of individuals, the celiac artery and the SMA arise from the aorta as a common trunk. In such cases, the common trunk splits into the celiac artery and the SMA within 1 or 2 cm from the aorta.1,2
Ultrasound examination of the celiac artery usually begins with a transverse sweep of the proximal abdominal aorta. The transverse approach allows visualization of the bifurcation of the hepatic and splenic branches, usually resembling a T or “seagull” (Figure 26-2, A). The longitudinal approach is preferred for evaluation of the celiac artery origin. We also utilize the longitudinal view for Doppler interrogation of the celiac artery. Consistent angle correction of greater than or equal to 60 degrees is obtained in this projection. This view also permits evaluation of the SMA, which is found just inferior to the celiac artery.
The characteristic Doppler waveform is a low-resistance arterial waveform (Figure 26-2, B). As mentioned above, continuous forward flow throughout diastole is required for adequate perfusion of the liver and spleen. The hepatic and splenic branches will also demonstrate the low-resistance pattern.3
The mesenteric circulation is notable for extensive arterial anastomoses and rich collateral network. This network allows for continuous circulation to the splanchnic vessels in the event of stenosis or occlusion of mesenteric branches, avoiding significant ischemic insult. With occlusion of the celiac artery, there is collateralization through the pancreaticoduodenal arterial arcade, a network of small vessels surrounding the pancreas and duodenum. These vessels enlarge and feed into the gastroduodenal artery. When the celiac is occluded, there is retrograde flow through the gastroduodenal artery to supply blood to the common hepatic artery. Thus, blood supply to the liver and spleen can be maintained.4
Splenic Artery
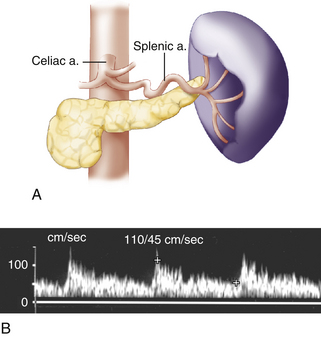
The splenic artery (limb of the celiac T toward patient’s left) follows a tortuous course along the posterosuperior margin of the pancreatic body and tail (Figure 26-3, A) and terminates by splitting into a number of branches in the hilum of the spleen. Along the way, the splenic artery gives rise to several pancreatic branches, short gastric branches, and the left gastroepiploic artery. These vessels are usually not seen with ultrasound. Transverse scans from a midline approach usually reveal the proximal portion of the splenic artery (see Figure 26-2, A). The distal portion of the splenic artery is best seen through the splenic hilum from a left lateral approach. Because of the tortuous course of the splenic artery, flow in this vessel is typically turbulent, (Figure 26-3, B).
Hepatic Artery
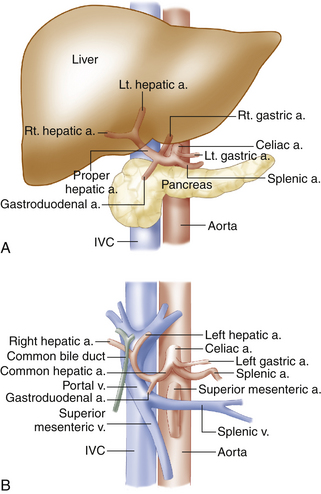
The common hepatic artery (Figure 26-4) is the limb of the celiac T that heads toward the patient’s right. After running a short distance along the superior border of the pancreatic head, the common hepatic artery gives rise to the gastroduodenal artery, which can often be seen with ultrasound at the anterosuperior border of the pancreatic head. Beyond the gastroduodenal artery origin, the common hepatic artery becomes the proper hepatic artery, which follows the portal vein to the porta hepatis. At this point, it divides into the left and right hepatic arteries, which penetrate into the hepatic substance. The anatomic relationships among the hepatic artery, the portal vein, and the extrahepatic bile ducts are shown in Figure 26-4, B.
The classic hepatic artery configuration just described is seen in 72% of individuals.5 A number of alternative patterns may occur, the most noteworthy of which are the following: (1) the common (4%) or right (11%) hepatic artery may arise from the SMA, and (2) the left hepatic artery may arise from a shared trunk with the left gastric artery (10%).2
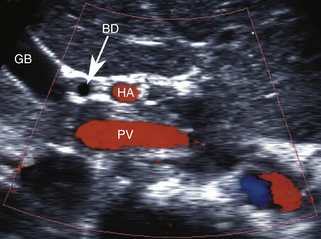
The hepatic arteries are usually well visualized sonographically from an anterior abdominal approach. The common hepatic artery is most easily identified at its origin from the celiac artery (see Figure 26-2, A). The proper hepatic artery is seen on ultrasound images near the porta hepatis, anterior to the portal vein, in short- or long-axis views, as can be seen in Figure 26-5. The right and left hepatic artery branches can be followed into the substance of the liver to a variable distance from the porta hepatis. As noted previously, the hepatic arterial system has low-resistance flow characteristics, with continuous forward flow throughout diastole. It is interesting to note that blood flow in the proper hepatic artery and portal vein are both hepatopetal, delivering blood flow toward the liver.
Superior and Inferior Mesenteric Arteries
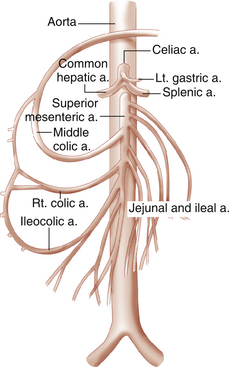
The SMA arises from the anterior surface of the aorta, immediately distal to the origin of the celiac artery (Figure 26-6). The SMA generally consists of a short, anteriorly directed segment and a much longer inferiorly directed segment that ends in the vicinity of the ileocecal valve. SMA branches supply the jejunum, ileum, cecum, and ascending colon, as well as the proximal two-thirds of the transverse colon and portions of the duodenum and pancreatic head. As noted previously, the SMA may also give rise to an aberrant right hepatic artery (11%) or common hepatic artery (4%).1 The SMA communicates with the celiac artery via the pancreaticoduodenal arcade.
The SMA is easily identified on longitudinal or transverse ultrasound images (Figure 26-7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree