Fig. 1
Different macroscopical types of cholangiocarcinomas. a the mass forming type. b the periductal infiltrating type. c the mixed type
2.
The periductal infiltrating type (PI), characterized by a tumoral growth spreading along intrahepatic portal tracts, associated with stenosis of the involved ducts and upstream bile duct obstructive dilatation and cholangitis (Fig. 1b).
3.
The intraductal-growing type (IG), defined as a polypoid or papillary tumor mass growing within the lumen of a dilated large bile duct.
Among these forms, the MF type is the most prevalent gross type, accounting for about 65 % of all ICC types, while PI type and IG type are rare, representing 6 and 4 % of all ICC, respectively. The predominant mixed pattern (around 25 % of ICC) combines to the PI type.
ICC originating from malignant transformation of peripheral ductules and small portal bile ducts usually results in a MF type with no connection with a bile duct macroscopically visible, while perihilar segmental ducts may result in any of the four types and are often associated with intrahepatic biliary fibrosis and cholangitis in the surrounding liver parenchyma. ICC from large intrahepatic bile ducts are often associated with noninvasive intraductal papillary neoplasm (IPN), which may result in mixed pattern, combining a MF to a IG type and extend superficially along the surrounding bile duct epithelium.
At advanced stages, intrahepatic metastases appear consisting on various sized nodules, which may coalesce; regional lymph nodes as lung metastases may develop.
2.1.2 Microscopic Pattern
Histologically, ICCs were, until recently, classified in classic adenocarcinomas and rare histological variants such as adenosquamous and squamous carcinoma, mucinous carcinoma (often with mucin visible at cut surface and intraductal growth pattern, occasionally associated with intestinal-type goblet cells), signet-ring cell carcinoma, clear cell carcinoma (with abundant cytoplasm), lymphoepithelioma-like carcinoma, and neuroendocrine type or may have sarcomatous area, mimicking a spindle cell sarcoma (Table 1).
Table 1
Classifications of intrahepatic cholangiocarcinoma
Traditional classification | New classification of ICC |
|---|---|
Adenocarcinoma | Adenocarcinoma conventional type |
Well differentiated | Well differentiated |
Moderately differentiated | Moderately differentiated |
Poorly differentiated | Poorly differentiated |
Adenocarcinoma unconventional type | |
Trabecular | |
Perihilar | |
Ductular | |
Rare variants | Rare variants |
Squamous cell type | Squamous cell type |
Adenosquamous cell type | Adenosquamous cell type |
Mucinous carcinoma | Mucinous carcinoma |
Signet-ring cell carcinoma | Signet-ring cell carcinoma |
Clear cell carcinoma | Clear cell carcinoma |
Sarcomatous carcinoma | Sarcomatous carcinoma |
Based on recent knowledge in carcinogenesis of CC, notably the existence of cholangiocytes’ heterogeneity along the different levels of the biliary tree and the role of hepatic stem cell (HSC), additional histological classifications of ICC have been proposed. These include subdividing ICC in conventional subtype (most often occurring without underlining liver disease) and unconventional subtype (most likely developing on the background of a non-biliary chronic liver disease and cirrhosis) or in mucin-producing or non-producing CC [3–6].
Histologically, conventional ICC is classic mucin-producing adenocarcinomas with biliary features and displays three major (occasionally overlapping) architectural patterns (Fig. 2):
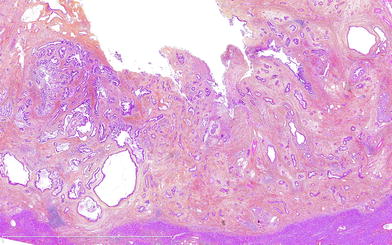
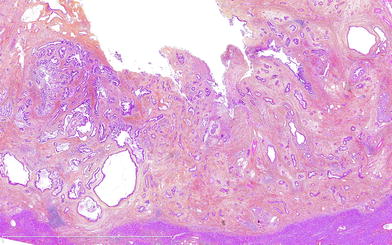
Fig. 2
Microscopical pattern of a well differentiated CC composed of tubular glands and abundant desmoplastic stroma along a large intrahepatic bile duct
1.
Well-differentiated fairly regular tubular glands with lumen of variable size, with or without micropapillary features. Tumoral cells are only slightly atypical and pleomorphic; they look like bile cells with small-to-medium size, cuboidal shape, with small nuclei and nucleoli surrounded by pale and occasionally vacuolated cytoplasm. Occasionally, neutrophil aggregates are intermingled within the tumoral glands.
2.
Moderately differentiated, more irregular, and tortuous tubular glands. Tumoral cells are mostly columnar shaped and moderately pleomorphic with a hyperchromatic nuclei and regular mitotic figures, surrounded by an eosinophilic cytoplasm.
3.
Poorly marked irregular glands or solid, nested, or cribriform growth pattern, occasionally associated with tumor necrosis. Tumoral cells are small and monomorphic cells with scanty cytoplasm and dark nuclei.
For unconventional ICC, several histological subtypes (both at architectural or cytological level) have been newly defined and subject to intense studies notably on their histogenesis.
1.
Trabecular subtype, made of polygonal eosinophilic tumoral cells arranged in thick, occasionally anastomozing trabeculae, mimicking an HCC. They however differ from HCC by indistinct nucleoli, absence of bile production, presence of central fibrosis with sparse tumoral cells, presence of calcification, and immunostaining characteristics.
2.
Hilar subtype mimicking typical hilar extrahepatic BDC. Large bile duct shows luminal spread of carcinoma and ulceration surrounded by periductal invasion similar to conventional ICC; peribiliary glands are often invaded. It most likely corresponds to CC originating from large bile ducts that have progressed into MF CC, peribiliary gland carcinoma, or a conventional ICC with secondary involvement of intrahepatic large bile ducts.
3.
Intraductal neoplasia of the intrahepatic bile duct
(a)
IPN of bile duct, characterized by a spectrum of lesion ranging from preneoplastic intraductal papillary neoplasm of the bile duct (IPNB) (see below) to well-differentiated papillary, noninvasive and invasive, adenocarcinoma. The invasive component often is a mucinous carcinoma. They typically correspond macroscopically to the intraductal growth type, and intraductal superficial intraepithelial tumoral spread may occur along large and even small bile ducts.
(b)
Intraductal tubular neoplasm of bile duct (ITBN), rare and principally composed of tumor tubular glands, rarely papillary, without mucin, that cast and obstructs the dilated biliary duct.
(c)
Superficial spreading type.
4.
Cholangiolocellular carcinoma (CLC), composed of proliferation of very regular and well-differentiated ductular structures within fibrosis, mimicking a ductal plate malformation [7]. It was previously categorized into a subtype of ICC (bile ductular adenocarcinoma) and is still as yet in Japanese literature. Today, because it is thought to originate from the hepatic progenitor cells (HPCs) located in ductules/canals of Hering [8, 9], it is classified in the latest edition (2010) of WHO tumor classification as a subtype of CHC and will be treated in that section (see below).
5.
ICC with predominant “ductal plate malformation” pattern characterized irregularly dilated neoplastic glands associated with an important desmoplastic fibrosis.
A general hallmark of ICC is histological heterogeneity (which may be responsible for misclassification at preoperative biopsy because of sampling problem) and an often, abundant desmoplastic fibrosis, variably distributed within the tumor. The center is often more densely fibrotic intermingled sparse tumoral cells, with occasionally focal calcifications. The periphery has more abundant and proliferating tumoral cells that infiltrate the surrounding parenchyma either by compression and infiltration along the sinusoids or by directly replacing hepatocytes in their cords. Portal tract is co-opted within the mass. Portal venules, lymphatic vessels, and intrahepatic nerves are often invaded, already at an early stage.
ICCs are positive at immunohistochemistry for biliary subtype of cytokeratin, namely cytokeratins 7 and 19, but no specific markers still exist in order to distinguish such tumors from HCC or metastases. ICC histological heterogeneity is also underlined by immunohistochemical profiles and gene expression profiling [1].
2.2 Extrahepatic Bile Duct Carcinoma
EBDC is defined as carcinoma arising either (1) from the common hepatic duct (proximal to cystic duct) to right or from left hepatic bile duct (segment assessed as extrahepatic from their junction in hepatic hilum up to the secondary bifurcation). This EBDC is also named hilar or Klatskin tumor or (2) from extrahepatic distal bile duct (segment distal to cystic duct), excluding ampulla of Vater.
2.2.1 Macroscopic Pattern
Distinguishing between perihilar ICC and hilar EBDC relies essentially on macroscopic examination and may be difficult or even arbitrary particularly at advanced stage. Peripheral ICC may have secondarily infiltrated large hilar bile duct, or on the contrary, a hilar EBDC may extend to form a mass with the liver parenchyma. This may explain some discrepancies in the literature notably concerning the epidemiology and incidence of this tumor.
Bismuth subclassification for Klatskin tumors is widely used for surgery. Type I tumor involves the common hepatic duct distal to the biliary confluence; type II tumor involves the biliary confluence; type IIIa tumor involves the biliary confluence plus the right hepatic duct; type IIIb tumor involves the biliary confluence plus the left hepatic duct; and type IV multifocal or tumor involves the confluence and both the right and left hepatic ducts.
According to their macroscopic appearance, BDC may also be further divided into four categories, with, beside the first one, often overlap between the types:
1.
The polypoid type (Fig. 3a), with endoluminal mass.
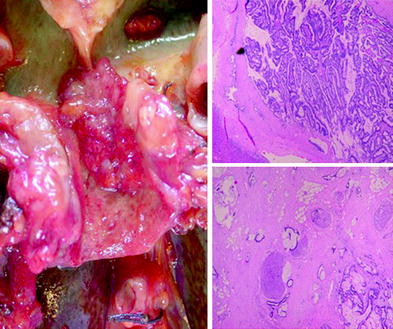
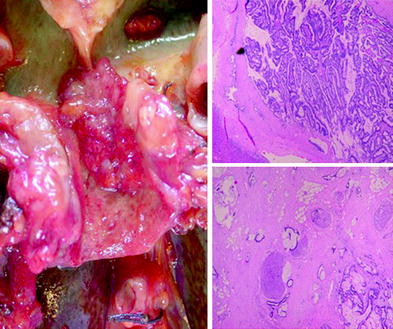
Fig. 3
a Macroscopical polipoïd types of extrahepatic bile duct carcinoma. b Microscopical papillary pattern of a moderate differentiated carcinoma, with c invasive component
2.
The sclerosing (scirrhous) constricting type, the most common, characterized by diffuse bile duct thickening due to extensive tumor infiltration and fibrosis spreading in periductal tissue.
3.
The nodular type.
4.
The diffusely infiltrating type, spreading linearly along the wall of the bile duct.
2.2.2 Microscopic Pattern
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree