Osteoid osteoma . (a) Homogeneous lucent lesion centered on the femoral cortex, representing osteoid osteoma. (b) Treatment was performed with CT-guided RF ablation
Nuclear Medicine
A radionuclide bone scan may demonstrate the double-density sign, which is related to increased vascularity.
Fine Needle Aspiration
Findings in aspirates of osteoid osteomas are relatively nonspecific. Numerous osteoblasts and osteoclasts are typically seen.
Osteoblasts are characterized by abundant granular cytoplasm, eccentric nuclei, and an area of cytoplasmic clearing opposite the nucleus and adjacent to the cell membrane.
Osteoclasts are multinucleated giant cells with low to intermediate nuclear:cytoplasmic ratios and round cell borders.
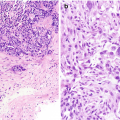
Core Biopsy
Cases of osteoid osteoma are characterized in histologic sections by delicate trabeculae of woven bone with osteoblastic rimming and scattered osteoclasts. The trabeculae are separated by richly vascular stroma composed of fibroblasts and loose collagen [3].
The centrally placed nidus is made up of thicker and more sclerotic bone.
Osteoblastoma
Clinical
Osteoblastomas are clinicopathologically similar to osteoid osteomas, but they are larger and are accompanied by less intense pain that is not relieved by salicylates.
Plain Radiograph
Osteoblastoma has a similar appearance to osteoid osteoma, but the lesions are generally larger than 2 cm.
Osteoblastomas are round or oval and may contain an internal matrix [8].
Nuclear Medicine
Osteoblastomas demonstrate methylene diphosphonate avidity.
Fine Needle Aspiration
Findings in aspirates of osteoblastoma are relatively nonspecific. Numerous osteoblasts and osteoclasts are typically seen [9].
Osteoblasts are characterized by abundant granular cytoplasm, eccentric nuclei, and an area of cytoplasmic clearing opposite the nucleus and adjacent to the cell membrane.
Osteoclasts are multinucleated giant cells with low-to-intermediate nuclear:cytoplasmic ratios and round cell borders.
Core Biopsy
Cases of osteoblastoma are characterized in histologic sections by delicate trabeculae of woven bone with osteoblastic rimming and scattered osteoclasts. The trabeculae are separated by richly vascular stroma composed of fibroblasts and loose collagen.
Areas of sclerosis and chondroid matrix formation may be seen in addition to osteoblasts with bizarre nuclei.
Correlation with radiographic findings is critical in order to exclude osteosarcoma.
Osteosarcoma
Clinical
In contrast to chondrosarcoma, osteosarcoma tends to occur in a bimodal distribution with peaks in the second decade as well as later in life.
Secondary osteosarcoma can occur in the context of radiation, Paget disease, and bone infarction.
Osteosarcoma most commonly affects the long bones in the lower extremities.
Osteosarcomas are characterized by the production of an osteoid matrix both pathologically and in radiographic studies.
Metastatic disease is not uncommon in the setting of high-grade osteosarcoma.
Plain Radiograph
Typically, osteosarcoma manifests as a long-bone, metaphyseal lesion with aggressive features. These include mixed areas of lysis and sclerosis, cortical destruction, periosteal new bone, and soft-tissue mass (Fig. 10.2) [10].
While there are eight subtypes of osteosarcoma according to the World Health Organization, conventional osteosarcoma is the most common and demonstrates cloudlike bone formation in the intramedullary space [11].
Osteosarcomas may also arise from the periosteum, in which case they are termed juxtacortical osteosarcomas.

Osteosarcoma . (a) Frontal radiograph of the knee demonstrating an aggressive lesion with cortical destruction, periosteal reaction, and osteoid matrix. Pathologic analysis confirmed the diagnosis of osteosarcoma. Coronal T1 (b) and coronal T2 (c) images demonstrate the extent of cortical breakthrough and soft-tissue extension to better advantage. The mass effect on adjacent structures is also better evaluated on MRI
Magnetic Resonance Imaging
MRI is useful for demonstrating the extent of soft-tissue involvement.
The extent of involvement of the medullary canal is also better shown on MRI.
Fine Needle Aspiration
Aspirates of osteosarcoma may have a variety of morphologic appearances.
While the majority of tumors contain frankly malignant pleomorphic tumor cells in epithelioid and/or spindle cell forms, lower grade tumors may be morphologically bland.
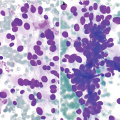
In cases of osteoblastic osteosarcoma, an osteoid matrix is present in the background or interspersed between tumor cells. The osteoid matrix is hyaline or densely fibrillary and metachromatic (magenta) on the Diff-Quik stain (Fig. 10.3a) [12].
In cases of chondroblastic osteosarcoma, chondroid matrix (metachromatic and less dense than the osteoid matrix) will be present [13].
In fibroblastic osteosarcoma, matrix may be absent. In these cases and particularly in small biopsies, the radiographic impression is key to allow the distinction from chondrosarcoma and malignant fibrous histiocytoma.
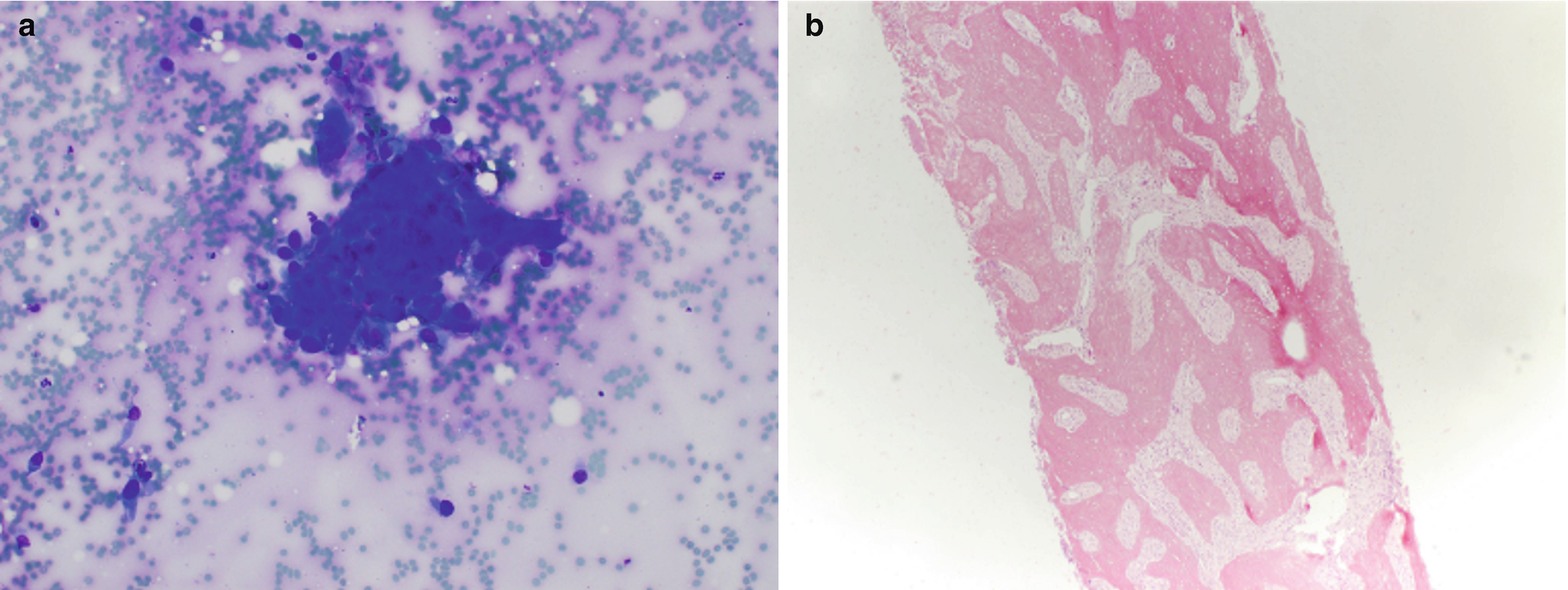
Osteosarcoma . (a) Polygonal tumor cells with delicate lacy osteoid matrix are seen in this aspirate specimen. (b) In histologic sections, thick trabeculae of woven bone are seen in a fibroblastic background
Core Biopsy
The appearance of osteosarcoma in histologic sections varies greatly, depending on the grade of the tumor and the degree of differentiation. Typical high-grade osteoblastic osteosarcoma is composed of frankly malignant tumor cells intimately admixed with a lacy osteoid matrix. Lower-grade tumors may have thickened bony trabeculae and be cytologically bland (Fig. 10.3b). In these cases, correlation with radiographic findings is critical in suggesting the correct diagnosis.
In chondroblastic osteosarcoma , a cartilaginous matrix is present and punctuated by lacunae. In cases of fibroblastic osteosarcoma, the tumor is morphologically identical to a pleomorphic undifferentiated sarcoma of soft tissue in that a matrix may be entirely lacking.
Chondroid Tumor Matrix: Osteochondroma, Enchondroma, Chondroblastoma, and Chondrosarcoma
Osteochondroma
Clinical
Osteochondromas are the most common benign bone tumors.
Complications of osteochondroma are typically related to mass effect, including vascular compromise, muscular or bursal irritation, or neurologic sequelae [14]. However, malignant degeneration may also occur, with transformation into chondrosarcoma.
Plain Radiograph
The majority are located about the knee or proximal humerus.
Osteochondromas are exophytic, typically metaphyseal lesions and may be sessile (broad-based) or pedunculated. They demonstrate continuity of the periosteum, cortex, and marrow with the underlying bone with an overlying cartilage cap (Fig. 10.4).
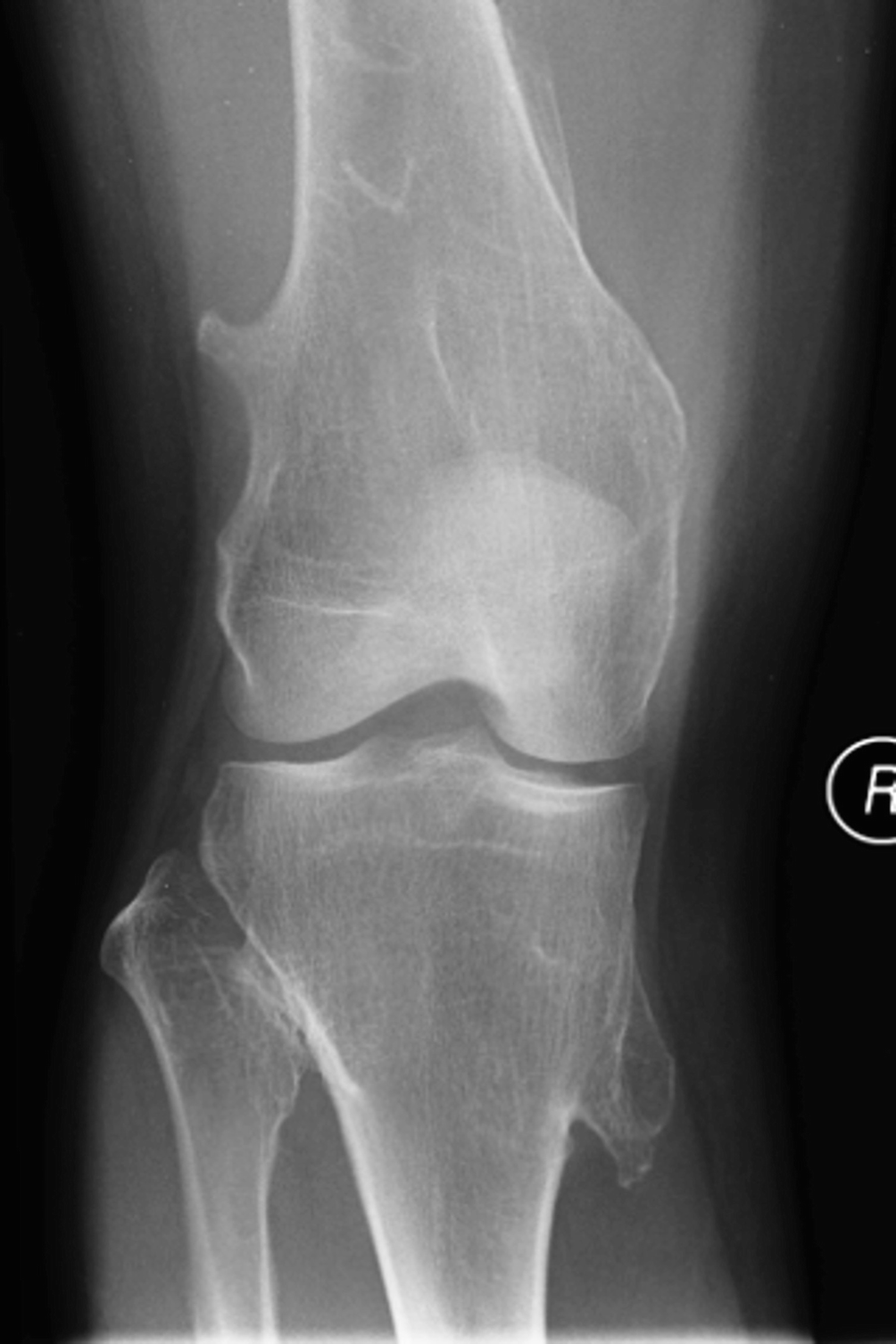
Osteochondroma . Frontal radiograph of the knee demonstrating multiple osteochondromas as pedunculated exostotic lesions arising from the metaphyseal regions about the knee. Multiple osteochondromas have a higher risk of malignant transformation to chondrosarcoma
Magnetic Resonance Imaging
MRI demonstrates the continuity of the osteochondroma with the underlying bone as well as the cartilaginous cap.
Complications related to mass effect are well appreciated on MRI [15].
Transformation to chondrosarcoma is a well-documented complication, and this risk correlates with a cartilage cap thickness greater than 2 cm. This is reproducibly measured on MRI. Cartilage cap thickness is measured from the junction of the T2 low-signal intensity mineralization with the near-fluid signal intensity cartilage to the surface of the cartilage, ignoring the undulations in the interface between them [16].
Fine Needle Aspiration
Osteochondromas do not typically yield cellular aspirates because they are predominantly made up of mature hyaline cartilage and bone. Aspirates may contain bone marrow elements and fragments of cartilaginous or bony matrix.
Core Biopsy
Findings in core biopsy depend on which portion of the lesion is sampled. The underlying bony stalk is made up of trabecular bone and typically contains normal bone marrow elements.
The cartilaginous cap is composed of mature hyaline cartilage that may display some degree of myxoid degeneration. The interface between the cartilaginous cap and the bony stalk is characterized by active enchondral ossification.
Enchondroma
Plain Radiograph
Enchondromas present as well-marginated medullary lucencies. The most commonly affected locations include the hands and feet as well as the femur, humerus, and tibia.
Lesions usually arise near an epiphysis and cause osseous expansion with endosteal scalloping and cortical thinning (Fig. 10.5).
These benign lesions often demonstrate a typical internal chondroid matrix superimposed on a background of lucency. This may involve minimal stippling to larger areas of heterogeneous density [17].

Enchondroma . Frontal radiograph of the distal femur demonstrating the classic appearance of an enchondroma, with a lucent lesion containing a central ring-and-arc chondroid internal matrix
Computed Tomography
Enchondromas demonstrate typical lobulated margins and an internal chondroid matrix.
Lesion size can be accurately assessed by CT.
CT helps to separate enchondromas from chondrosarcomas by better demonstrating other aggressive features, such as cortical destruction or periosteal reaction. Enchondromas typically measure less than 5 cm in greatest dimension [7].
Fine Needle Aspiration
Aspirates contain a metachromatic fibrillary chondroid matrix with clear round lacunae with bland round chondrocytes
Core Biopsy
Lesions are characterized by hyaline cartilage containing bland chondrocytes in the lacunae.
Myxoid change, increased cellularity, and cytologic atypia suggest malignancy but may be pronounced in enchondromas involving the small bones of the hands and feet [12].
Enchondromas are almost invariably circumscribed lesions without permeation of the trabeculae.
Chondroblastoma
Clinical
RF ablation has been described as an alternative to surgery for some cases of chondroblastoma , depending on the risk of mechanical collapse and lesion size [18].
Plain Radiograph
Chondroblastomas demonstrate geographic bone destruction with well-defined margins [19].
Lesions are centered at the epiphysis in tubular long bones.
Magnetic Resonance Imaging
Chondroblastomas demonstrate low to intermediate T1 signal and T2 heterogeneity [20].
Postcontrast images demonstrate mild tumoral enhancement.
Adjacent soft-tissue and bone marrow edema may also be present.
Fine Needle Aspiration
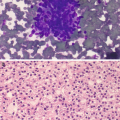
These tumors are characterized by a triphasic appearance.
Polygonal mononuclear cells with bland, grooved nuclei predominate. These cells are characterized by dense cytoplasm and may contain hemosiderin pigment [21].
Osteoclast type giant cells.
Fragments of a metachromatic fibrillary or amorphous chondroid matrix that may be calcified.
Core Biopsy
Chondroblastomas typically display sheets of polygonal mononuclear cells with relatively well-defined cell borders and uniform round nuclei that may be grooved and somewhat hyperchromatic (Fig. 10.6). Scattered throughout are multinucleated osteoclast-like giant cells. Interstitial “chicken wire” calcifications and a chondroid matrix may be present and allow distinction from other giant cell rich lesions such as aneurysmal bone cyst and giant cell tumor of bone.
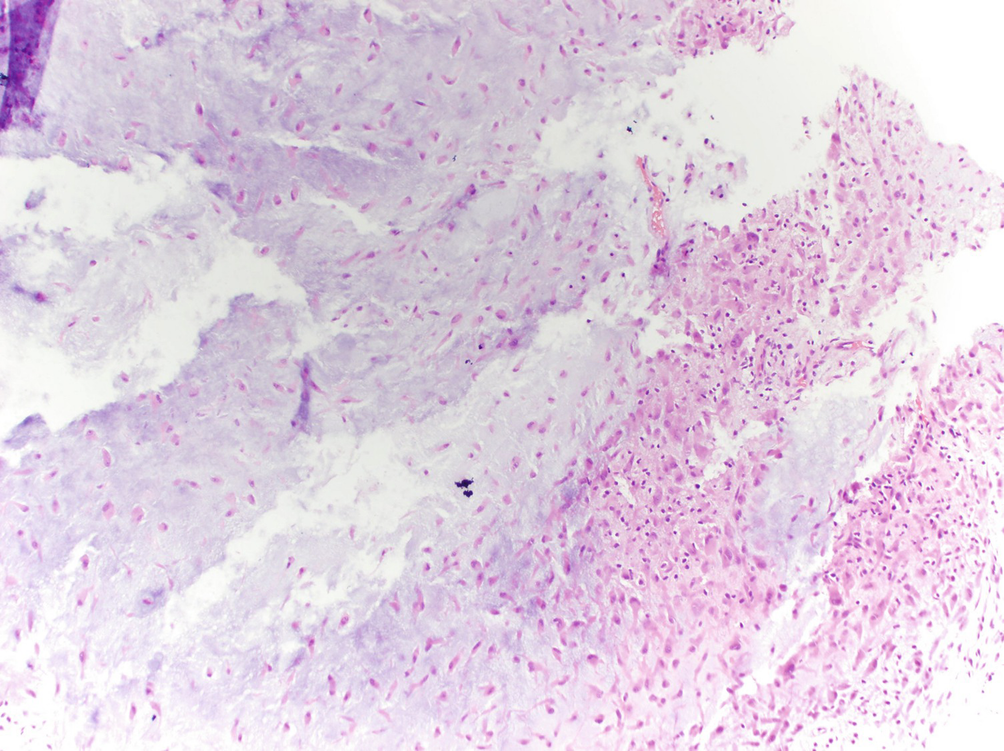
Chondroblastoma . Histologic sections show lobules of chondroid matrix with bland spindled cells reminiscent of chondromyxoid fibroma. At the periphery are more cellular areas composed of polygonal cells with interspersed giant cells
Chondrosarcoma
Chondrosarcoma
Chondrosarcomas most frequently involve long bones and occur in older individuals. Although these tumors may grow large and be locally advanced, metastatic spread is less common than in other sarcomas.
Secondary chondrosarcoma may occur in the settings of Ollier and Mafucci syndromes, synovial chondromatosis, and preexisting osteochondroma.
Plain Radiograph
While there is occasionally overlap with features seen in enchondromas, chondrosarcomas typically demonstrate aggressive features that include cortical destruction, periosteal thickening, and endosteal scalloping (Fig. 10.7) [22].
Lesions may include mixed lytic and sclerotic regions, with periosteal reactions ranging from thick, unilaminar, more benign-appearing periosteal reaction to a spiculated, aggressive appearance.
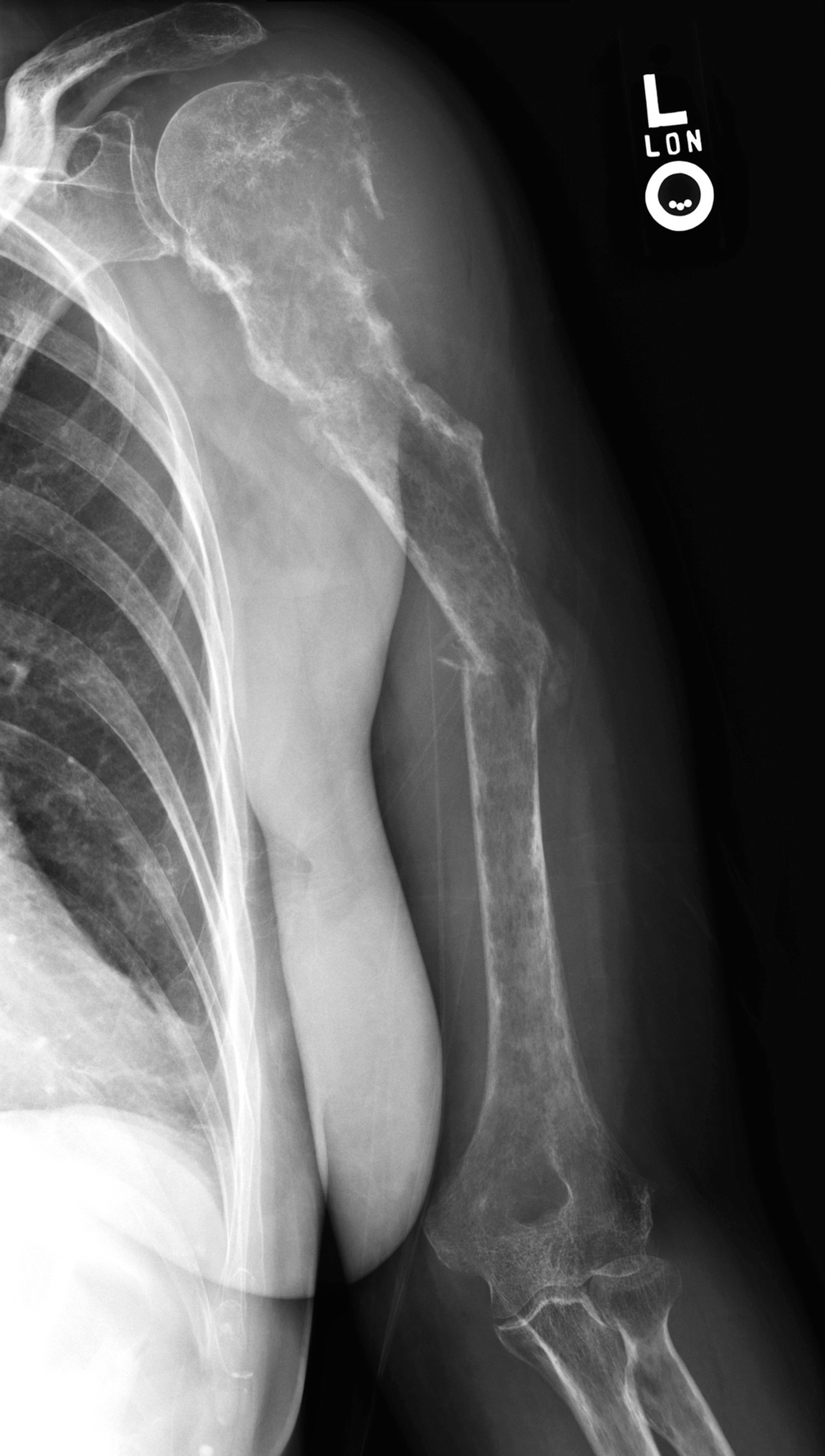
Chondrosarcoma . Radiograph of the humerus demonstrates a chondroid matrix with diffuse cortical destruction and a lesion size much greater than 5 cm. Pathologic analysis confirmed the diagnosis of chondrosarcoma. Compare with the benign-appearing enchondroma in Fig. 10.5
Magnetic Resonance Imaging
Classicly, a chondroid matrix of a chondrosarcoma appears as alternating high T2 signal intensity lobules with heterogeneous areas of low T2 signal intensity. The low T2 signal intensity areas represent areas of calcification within the matrix.
The extent of soft-tissue involvement is much better delineated on MRI.
Larger lesion size correlates with a higher likelihood of malignancy.
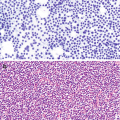
Fine Needle Aspirates
Aspirates are characterized by malignant chondrocytes within lacunae accompanied by an abundant chondroid matrix [23].
Chondrocytes are typically round cells with abundant clear to granular cytoplasm and round nuclei. They reside within rounded spaces (lacunae) within the chondroid matrix of the tumor.
The chondroid matrix is intensely metachromatic, with varying degrees of myxoid and fibrillary change.
The degree of cytologic atypia impacts the overall morphologic picture. Cases of low-grade chondrosarcoma are morphologically indistinguishable from chondroma in aspirates. High-grade chondrosarcomas, in contrast, may contain little matrix and may be composed of sheets of overtly malignant cells.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree