Considering the awesome aspect of the therapy machines together with the fact that no one may be with the patient during the period of irradiation, it is surprising that the great majority submit to the complete course of therapy with little or no restraint and no sedation…. In a small number of patients in the infant-to-toddler age group of 11/2 to 5 years of age, patient cooperation may be impossible to obtain…. Complete immobility of the patient is absolutely essential for the accuracy and success of treatment…. Sedation of the patient becomes virtually a sine qua non.
Harrison and Bennet (
1) made these observations more than 30 years ago. Their classic article, “Radiotherapy Without Tears,” was the first published report describing anesthesia for radiotherapy in children. The problem of inadequate sedation prompted the authors to develop
the following simple method of anesthesia for radiotherapy of infants…. The method is applicable when the anesthetist remains outside the treatment room and consists of the insufflation of nitrous oxide, oxygen, and halothane through the sidearm of the oropharyngeal airway (
1).
Forty years of progress in anesthesiology have validated not only Harrison and Bennet’s observation but also their solution to the problem of providing anesthesia for radiotherapy. This chapter reviews issues in the sedation of children with an emphasis on monitoring the anesthetized child in the radiotherapy suite, develops a model of the ideal anesthetic for pediatric radiotherapy, explores anesthetic options for radiotherapy, and discusses the implications of the child’s underlying disease that influence the anesthetic choice.
BEHAVIORAL TECHNIQUES TO AVOID ANESTHESIA
When possible, children should be irradiated without anesthesia. In some cases, a behavioral program to teach children how to cooperate with radiation treatment without sedation and anesthesia may be successful. Behavioral therapy techniques, called desensitization or exposure therapy, were originally developed for treating severe anxiety, fears, and phobias. The procedure involves inducing a relaxed state using music, cartoons, stories, or videos. Subsequently, one introduces the staff, equipment, and routines needed for radiation treatment.
A behavioral technique called differential positive reinforcement is used to strengthen cooperation and coping. Incentives such as praise, stickers, toys, and prizes are provided when the child attempts to cooperate. These are used to shape the child’s ability to inhibit movement when instructed to do so. Shaping is a behavioral psychology technique whereby the criteria for reinforcement are gradually altered as the child improves performance. At the beginning, an approximation of the desired behavior is acceptable. After a while, more challenging and rigid criteria are set for reinforcement.
Videotaped cartoons and movies may be used to provide relaxation, distractions, and ongoing positive reinforcement in training young children to cooperate with radiation therapy. A small television monitor can be suspended near the linear accelerator couch and connected to a VCR so that movies or cartoons may be played during radiotherapy while the child is in the treatment position. Slifer et al. (
2,
3,
4) demonstrated the efficacy of this technique in children between the ages of 21/2 and 7 years. Nine of 11 children were able to successfully undergo all of their radiation planning and treatment sessions without sedation.
The implementation of a psychoeducational intervention consisting of careful preparation of the patient for radiotherapy through the use of picture books, medical play, and reward systems reduced the need for anesthesia in a longitudinal study (
5). After implementing the intervention, the percentage of children requiring anesthesia decreased from 21% to 9%. The authors concluded that the cost of implementation (median 6 hours of time by a qualified nurse, plus materials) was offset by the reduced requirement for anesthesia.
Many pediatric radiotherapy centers have thoughtful programs designed to provide the services described above. Music therapists, psychologists, play therapists, social workers, and radiation therapists throughout the world have created a variety of culturally appropriate tools that they are almost always willing to share with colleagues including radiation therapy “comic books,” “coloring books,” video education tools, “make your own movie about radiotherapy with you as the star,” cheerful murals painted on the walls of the radiotherapy waiting room, and decorating stabilization devices with child-friendly themes. At meetings of professional societies these heart-warming ideas are freely shared with colleagues.
FREQUENCY OF ANESTHESIA FOR PEDIATRIC RADIOTHERAPY
When behavioral techniques to achieve patient cooperation and stability fail, anesthesia or sedation must be used. The frequency of anesthesia use as a function of patient age at the initiation of external beam radiation therapy in the Duke University Medical Center pediatric radiotherapy population is shown in
Table 21.1. For very young children (≤3 years) anesthesia is almost always needed. After approximately 5 years of age, however, anesthesia is rarely needed.
GOALS OF ANESTHESIA FOR RADIOTHERAPY
To accomplish the twin goals of irradiating the treatment volume while sparing healthy tissue, control of patient movement must be precise and absolute. How are these goals achieved in children? The approach varies depending on the institutional resources. Conscious or deep sedation is used in some centers, whereas general anesthesia is used in others. Regardless of the institutional practice, there is no substitute for vigilant monitoring and prompt intervention by people skilled in detecting and managing complications associated with the administration of sedative drugs to infants and children.
Anesthesiologists are increasingly asked to provide care outside the traditional operating room setting, such as in the radiotherapy suite. This is appropriate because the specialty has unique expertise in patient evaluation, selection, and monitoring and the ability to respond immediately to any complication of therapy. Expertise in drug selection and a comprehensive approach to the care of the child, which includes preanesthetic evaluation, postanesthetic care, and the provision of up-to-date feeding guidelines, are hallmarks of the anesthesiologist.
A prolonged fast before the induction of general anesthesia is no longer necessary. The American Society of Anesthesiology recommendations on preanesthetic fasting apply to all ages and are widely followed as standard of care (
6). All patients can safely drink clear liquids (e.g., apple juice, water, popsicles) until 2 hours before induction. Breast milk is allowed up to 4 hours, and milk or formula until 6 hours before induction. A light breakfast, for example toast and milk, may be allowed up to 6 hours prior to anesthesia for afternoon cases, but typically solid foods are withheld after midnight, especially in older children.
The goals of anesthesia for pediatric radiotherapy are listed in
Table 21.2. There are several options that, to varying degrees, accomplish the listed goals. There are no prospective,
randomized studies in the setting of pediatric radiotherapy that demonstrate the superiority of one technique of general anesthesia over another.
Several routes of drug administration are available for sedation of children. Each drug and drug combination has its own set of side effects and contraindications. Several general guidelines may be considered. First, the route of administration of the drug should be the least traumatic for the particular child. Oral administration, avoiding intramuscular or intravenous administration, should be considered when feasible. Second, it should be kept in mind that some children will develop a tolerance to certain drugs used for sedation. Over time, the amount of drug and time needed to achieve sedation may both increase.
INHALED ANESTHETICS
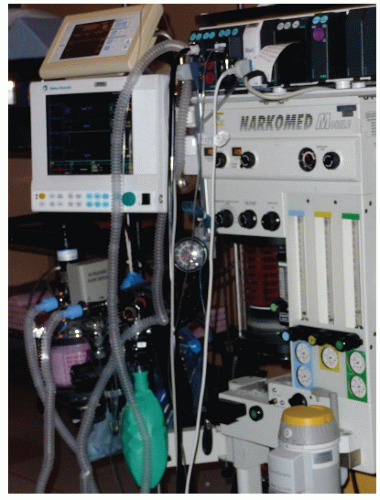
Several general anesthetic options exist for radiotherapy. The anesthesiologist individualizes therapy based on data obtained from the patient’s history, physical and laboratory examination, and discussions with the child, parents, and radiation oncologist. The physical limitations of the radiotherapy suite (such as the presence of an air exhaust system so that volatile anesthetic agents can be used) are also important in devising the anesthetic plan.
General anesthesia is accomplished with either inhaled agents (
Table 21.3) or intravenous agents (e.g., barbiturates, ketamine, propofol). The use of inhalational agents requires an anesthesia machine and, ideally, a waste scavenging system. The first report of anesthesia for pediatric radiotherapy used halothane. Halothane is a halogenated hydrocarbon volatile anesthetic first introduced for clinical use in 1956. Halothane has a long history of safe, effective use in pediatric patients. It rapidly produces an anesthetic state when inhaled, with minimal airway complications such as coughing and laryngospasm. Due to its tendency to depress cardiovascular function in a dose-dependent fashion and its arrhythmogenic potential, it has generally been replaced by sevoflurane for mask induction in children (
7). Sevoflurane has minimal pungency compared with halothane and may be more readily tolerated by children. Its lower solubility permits a more precise control over the delivery of anesthesia and a more rapid induction of and recovery from anesthesia. Sevoflurane also seems to have a lower respiratory irritant capacity than halothane and produces less coughing and breath holding than some other inhaled agents (
8,
9,
10,
11) (
Fig. 21.1).
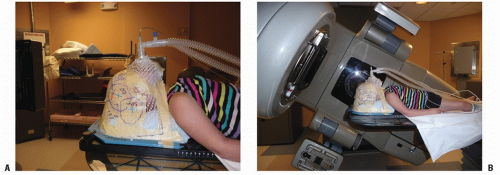
A risk of inhalation anesthesia is upper airway obstruction, which is often exacerbated in radiation therapy by the position of the patient. Positioning often entails immobilization of the child’s head in a stabilization device (
Fig. 21.2), which can impede airway patency (
Fig. 21.3) when an insufflation technique is used. This obstruction is relieved with an oropharyngeal or nasopharyngeal airway or a laryngeal mask airway (LMA). Although endotracheal intubation may be necessary in a small proportion of patients presenting for radiotherapy, it is preferable to avoid this technique because repeated laryngoscopy and intubation carry the risk of airway edema and trauma to the laryngeal structures. Intensity-modulated radiotherapy and tomotherapy techniques often allow the radiation oncologist to use a supine rather than a prone position for irradiation of the craniospinal axis, for example. Management of the airway in a supine patient is far easier for the anesthesiologist. This is an example of how the anesthesiologist and pediatric radiation oncologist can collaborate to ease each others contribution to the care of the child.
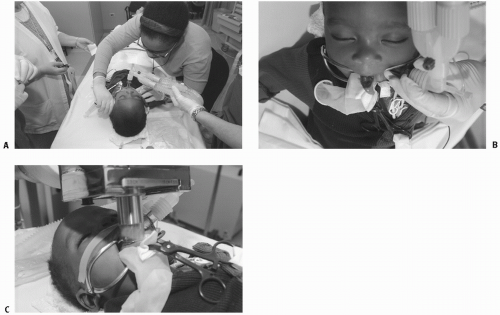
An adjunct for airway management during pediatric radiotherapy is the LMA. The LMA (
Fig. 21.4) is a silicone tube, the distal end of which has an elliptical-shaped cuff that, when correctly inserted and inflated, forms a low-pressure seal around the larynx and allows spontaneous ventilation in a variety of body positions without the need for endotracheal intubation. Therefore, the LMA provides many of the advantages of endotracheal intubation: a guaranteed patent airway without the disadvantages of repeated laryngoscopy and intubation. The LMA has been used for radiotherapy in children as young as 3 weeks of age. Grebenik et al. (
12) reported the use of the LMA for pediatric radiotherapy in 25 children who received more than 300 anesthetics. They observed no complications directly related to the use of the LMA. Morris and Marjot (
13) reported one case of posterior pharyngeal wall edema that corresponded to the area of contact between the posterior surface of the LMA and the oropharynx in a child repeatedly anesthetized with an LMA for radiotherapy. Moylan and Luce (
14) reported more than 2500 anesthetics given to 145 children with an LMA over a 4-year period for radiotherapy. They raised the concern that a prone position for radiotherapy with the neck partially flexed can produce kinking of the LMA, with the possibility of airway obstruction. A reinforced LMA may help alleviate this problem (
15).
In summary, general inhalation anesthesia has the following features that make it an attractive technique for pediatric radiotherapy: onset is rapid, depth is easily controllable, administration is not unpleasant, recovery is rapid, the incidence of nausea and vomiting is low, and airway patency is well preserved.