Clinical Presentation
The patient is a 65-year-old female with a history of chronic low back and neck pain and markedly reduced mobility in the cervical and lumbar region. Her records have noted the diagnosis of ankylosing spondylitis for 20 years. She has always been and remains HLA-B27 negative; 15 years ago she developed Crohn’s disease, which has been controlled with sulfasalazine (Azulfidine). Bilateral total hip replacement procedures were performed 13 years ago. She has recently become weak in both lower extremities and has developed peripheral neuropathy and bladder dysfunction. Physical examination reveals absent lower extremity reflexes and loss of position sense in both feet. Presumptive diagnosis of cauda equina syndrome was made.
Imaging Presentation
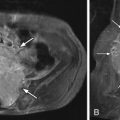
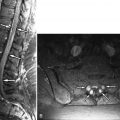
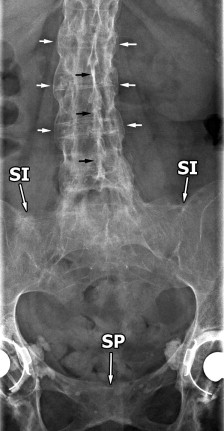
Anteroposterior (AP) and lumbar spine radiographs ( Figs. 8-1 and 8-2 ) reveal symmetric fusion of both sacroiliac (SI) joints and a bamboo configuration of the spine. The vertebral bodies have a squared off configuration and vertebral body syndesmophytes are visible at all lumbar and visualized lower thoracic levels. There is calcification of the intervertebral discs and posterior interspinous and supraspinatus ligaments. Syndesmophytosis and bilateral SI joint fusion are demonstrated on the radiographs and magnetic resonance (MR) images ( Figs. 8-1 to 8-5 ) . There is diffuse lumbar dural ectasia and multiple arachnoid diverticula eroding the lamina at several lumbar levels (see Figs. 8-4, 8-5; Fig. 8-6 ). The nerve rootlets are adherent to the posterolateral aspect of the thecal sac in and adjacent to the arachnoid diverticula giving a “vacant” thecal sac appearance consistent with chronic arachnoiditis. The intervertebral discs are heterogeneous on MR secondary to intradiscal calcification or ossification (see Figs. 8-2, 8-4, and 8-5 ).





Discussion
Ankylosing spondylitis (AS), also called Marie-Strümpell disease , is a seronegative (rheumatoid factor-negative) disorder causing sacroiliitis, enthesopathy, and spondyloarthropathy, with variable peripheral joint involvement. This is a complex, often debilitating condition with insidious onset and a variable degree of involvement in the spine. The socioeconomic impact of AS on the patient, her family, and on the healthcare system in general cannot be understated. Of all patients with ankylosing spondylitis, 95% are HLA-B27 positive compared with 8% of control white populations; 5% of patients with clinical and imaging manifestations of AS are HLA-B27 negative, as in the patient described earlier. HLA-B27 is a genetically encoded antigenic protein found on the surface of leukocytes in some persons. Approximately 1% of patients who are HLA-B27 positive will develop a rheumatoid factor–negative spondyloarthropathy (ankylosing spondylitis, psoriatic arthropathy, Reiter’s disease, and arthritis of inflammatory bowel disease). HLA-B27 is believed to play an important role in initiating and perpetuating the T-cell–mediated immune process, which leads to the manifestations of AS in most patients with this disorder. It has been postulated that some external antigenic agent, possibly a microbial agent, may trigger an abnormal response by T-cells to the HLA-B27/peptide complexes that form in these patients. Cytokines, such as interleukin-10, as well as genetic and environmental factors, are also believed to play a role. The resulting inflammatory cellular infiltrates target cortical bone, cartilage, and ligaments adjacent to fibrocartilaginous and synovial joints. Many of the manifestations of AS are the result of an exaggerated reparative response to this inflammatory process.
The prevalence of AS is between 0.2% and 0.8% in whites. AS occurs five times more commonly in men than in women. Juvenile ankylosing spondylitis can occur as well. AS disease progression tends to spread cephalad from the SI joints to the lumbar spine and eventually may involve the thoracic and cervical spine, although spinal involvement is variable and may not be contiguous. Women tend to have a milder course of disease progression, and spinal involvement has a tendency to be more discontiguous in women. Patients with AS usually present between the ages of 15 and 35 with severe low back or sacroiliac pain and stiffness of the spine and joints. The patient presents with low back pain or sacroiliac pain, back stiffness, and sometimes sciatic pain. Constitutional symptoms such as anorexia, weight loss, and low-grade fever may also be present. Patients who present later in life tend to have a better prognosis. Early onset of disease or involvement of the hip joints is usually associated with poor prognosis. With time, severe osteoporosis develops, and the paraspinal muscles tend to become atrophic because of disuse. The inadequately supported, brittle spine becomes very susceptible to spinal fractures, which can contribute significantly to the morbidity of these patients. It is important to be aware that cauda equina syndrome may occur in patients with AS. The etiology of cauda equina syndrome in patients with ankylosing spondylitis is controversial. Cauda equina syndrome may develop in AS patients in the absence of mass effect upon the cauda equina in AS patients. It has been postulated that in AS patients, arachnoid adhesions secondary to arachnoiditis, tether the cauda equina nerve rootlets to arachnoid diverticula. Inflammation of the arachnoid within these diverticula in AS patients has been described. Indeed, this could be the cause of the cauda equina syndrome in the patient presented above.
A discussion of the detailed clinical and radiographic criteria for diagnosis of AS is beyond the scope of this discussion but can be found elsewhere. Sacroiliitis is the hallmark of AS and usually occurs early in the disease. Initially, one SI joint may be more affected than the other, but as the disease progresses, the sacroiliac involvement characteristically becomes bilaterally symmetric. Ankylosing spondylitis begins as an erosive arthropathy affecting the synovial portions of the SI joints bilaterally and usually symmetrically. Erosions begin first on the iliac side of the SI joints and then involve both cortical surfaces of the synovial portion of the SI joints. The SI joint spaces widen, the adjacent cortical margins later become sclerotic, and eventually the SI joints fuse in a bilaterally symmetric fashion (see Fig. 8-3, Fig. 8-7 ). The fibrous portions of the SI joints may also be involved but usually do not fuse to the same degree as the synovial portions of the SI joints. Ankylosing spondylitis may be limited to the SI joints, but AS has a predilection for the axial skeleton, affecting fibrocartilaginous and synovial joints and adjacent vertebrae. The lumbar spine is often affected, but the thoracic and cervical spine may also be involved to a variable degree. Some portions of the spine may not be significantly involved. Sometimes AS affects the lumbar and cervical spine with relative sparing of the thoracic spine.

In AS, in the acute inflammatory phase, cortical bone damage occurs, and this phase is relatively short compared with the reparative and bone deposition phase. In the spine, this is manifested early on as an erosive arthropathy, which may involve synovial and fibrocartilaginous joints. The cortical erosions begin along the corners of the vertebral bodies at the discovertebral junction (Romanus lesions), most often beginning at the thoracolumbar junction, but can eventually progress to involve the entire spine. Sclerotic lesions often develop at the corner of vertebral bodies ( shiny corner sign). The erosions undergo a reparative process leading to adjacent sclerosis. The bone reparative response is not confined to the damaged cortex. The bone deposition continues to involve adjacent ligaments and the outer annulus of the disc, resulting in thin vertically oriented syndesmophytes ( Fig. 8-8 ) . The involved vertebral bodies typically develop a squared-off appearance, in part due to post erosive cortical sclerosis and also due to paraspinous ligamentous calcification and eventual ossification (see Figs. 8-2, 8-4, 8-5, and 8-8 ).

AS is an inflammatory enthesopathy (enthesitis), that is, an inflammatory condition that affects ligamentous and tendinous attachments in the spine, hips, and shoulders and sometimes affects the more peripheral appendicular joints. Paraspinous ligamentous abnormalities are very common, beginning early in the disease, and can represent a prominent manifestation of this disease.
In ankylosing spondylitis, early inflammation occurs where the outer fibers of the annulus fibrosus ( Sharpey’s fibers ) insert into the corners of the vertebral bodies. These outer annular fibers ossify along with thin ossifications of the paraspinal ligaments to form syndesmophytes, which are seen as thin vertically oriented ossifications of the anterior longitudinal ligament and lateral paraspinal ligaments that extend along the anterior and lateral vertebral body margins from mid-vertebral level to adjacent mid-vertebral level, in continuity with the ossified outer annular fibers of adjacent intervertebral discs (see Figs. 8-4, 8-5, and 8-8 ). This results in the so-called bamboo spine appearance (see Fig. 8-1 ). The syndesmophytes that develop in psoriatic and Reiter’s spondyloarthropathies tend to be larger, more exuberant, asymmetric bony excrescences arising along the discovertebral margins.
In ankylosing spondylitis, the zygapophyseal (facet) joints undergo an erosive arthropathy initially, but later become sclerotic and eventually fuse ( Fig. 8-9 ) . The vertebrae in AS are very brittle because of osteoporosis and are prone to fracture. The fractures are frequently transverse in orientation and may form pseudoarthroses. These pseudoarthroses may extend transversely through the vertebrae or through the intervertebral disc.